Yeast Infection: Causes, Symptoms, and Treatment
When dealing with Yeast Infection, a common fungal overgrowth that usually affects the vagina, mouth, or skin. Also known as Candidiasis, it often shows up as itching, discharge, or burning during urination. Understanding the basics helps you spot it early and act fast.
Key aspects to know
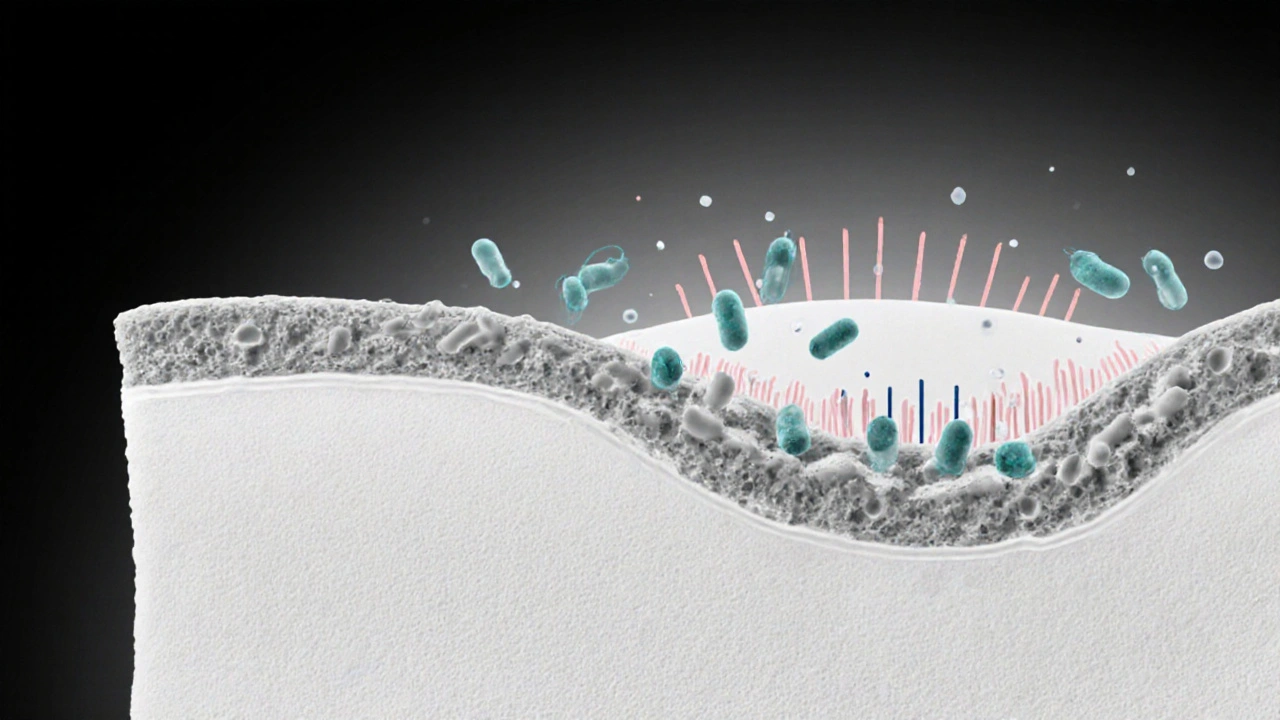
Antifungal Medication, drugs like fluconazole or clotrimazole that target Candida species is the mainstay of treatment, and yeast infection usually clears within a few days when used correctly. Vaginal Microflora, the balance of good bacteria and yeast that keeps the area healthy plays a preventive role; disruptions from antibiotics or hormonal shifts can tip the scales toward overgrowth. Risk Factors, conditions like diabetes, pregnancy, high estrogen levels, and tight clothing increase the chances of an episode. In short, yeast infection encompasses vulvovaginal candidiasis, requires antifungal medication, and is influenced by risk factors such as diabetes. Maintaining a healthy vaginal microflora helps prevent recurrence, while hormonal changes can trigger new flare‑ups.
Below you’ll find a curated mix of articles that touch on the same themes – from hormone‑related skin issues and pregnancy care to diabetes management and medication safety. Each piece offers practical tips you can apply right away, whether you’re trying to stop an outbreak, prevent future ones, or simply understand how your body’s chemistry affects infection risk. Dive in and discover the tools you need to stay ahead of yeast infection challenges.
How the Immune System Prevents and Fights Vaginal Infections
- Laura Ledas
- Aug, 22 2025
Learn how the immune system protects the vagina, why infections happen, and practical steps to strengthen your natural defenses.
Learn More