Every month the vagina faces a barrage of microbes, pH shifts, and hormonal changes. Yet most of the time we don’t notice a thing because the body’s natural defenses are hard at work. Understanding how the immune system protects this delicate environment can help you make smarter choices when things go wrong.
How the immune system a complex network of cells, tissues, and signals that defends the body against pathogens Keeps the Vagina Healthy
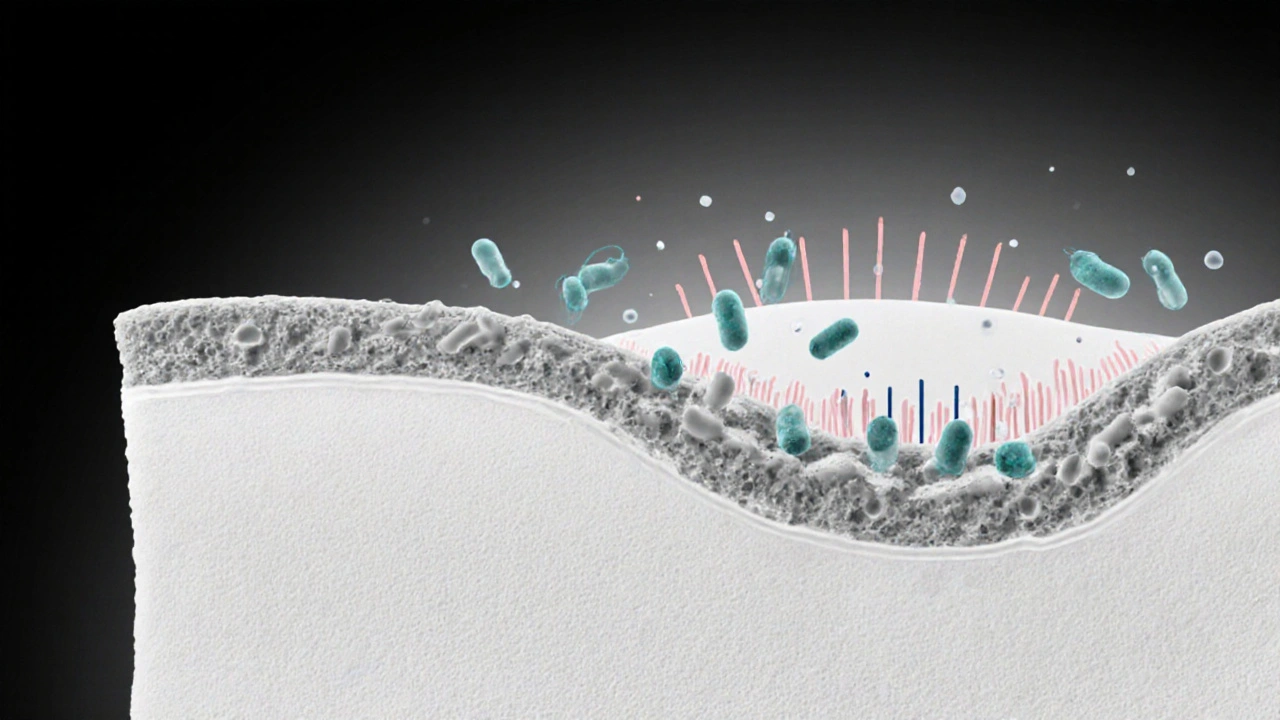
Vaginal health isn’t just about hygiene; it’s a partnership between the resident microbiome and the body’s defenses. The first line of protection is physical and chemical: the thin epithelial lining, natural acidity (average pH 3.5-4.5), and mucus that traps invaders. Lactobacillus species, the dominant bacteria, produce lactic acid and hydrogen peroxide, creating an environment that most harmful microbes can’t survive in.
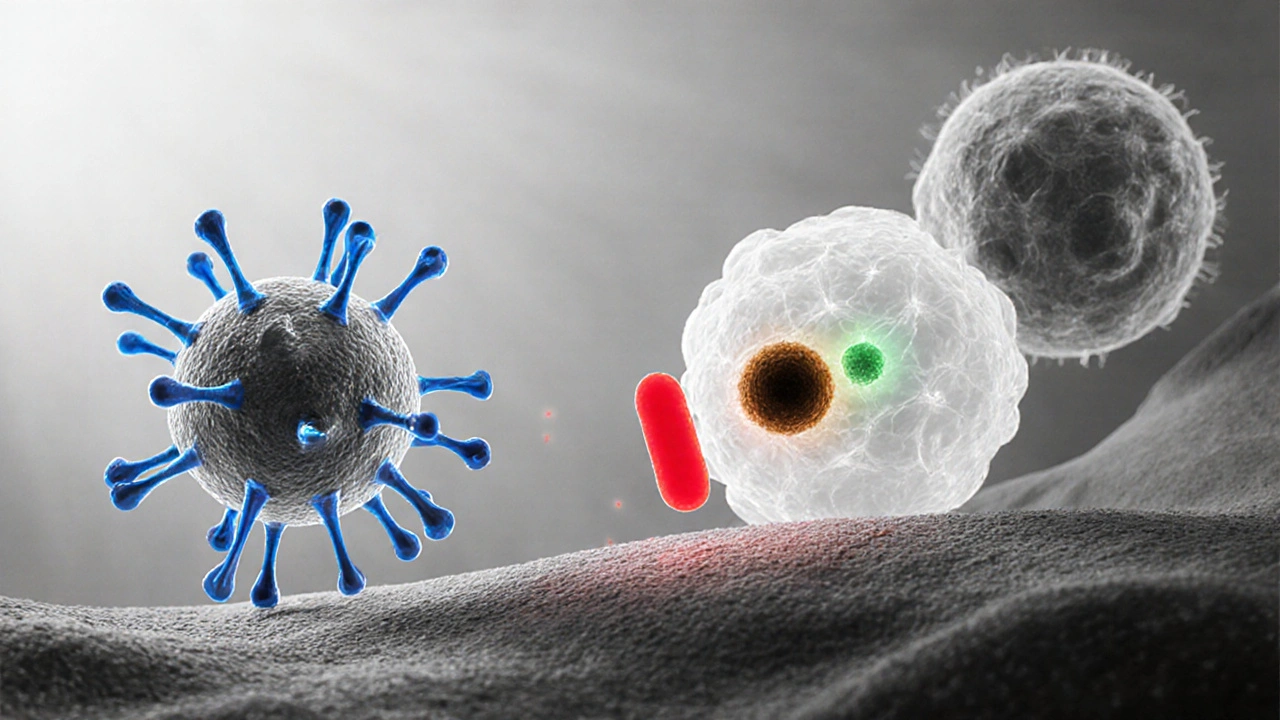
When a pathogen tries to break through, the innate arm of the immune system launches an immediate response. Pattern‑recognition receptors on epithelial cells detect bacterial wall components, triggering the release of antimicrobial peptides like defensins and cathelicidins. These small proteins punch holes in microbial membranes, neutralising them before they can multiply.
Key Players in Vaginal Defense
Beyond the barrier, several immune cells patrol the tissue:
- Neutrophils first‑responders that engulf and destroy bacteria
- Macrophages cells that ingest pathogens and signal other immune components
- Tcells adaptive immune cells that recognize specific antigens and coordinate a targeted attack
- Bcells produce antibodies that neutralise fungi and parasites
- Cytokines signalling proteins that orchestrate inflammation and healing
These cells communicate through cytokines such as interleukin‑1β and tumor necrosis factor‑α, which increase blood flow and recruit more defenders to the site of infection.
Common Vaginal Infections and the Immune Response
Three infections dominate clinical visits: bacterial vaginosis (BV), Candida (yeast) infection, and trichomoniasis. Each triggers a distinct immune pattern.
| Infection | Dominant Microbe | Innate Response | Adaptive Response | Typical Symptoms |
|---|---|---|---|---|
| Bacterial Vaginosis | Gardnerella vaginalis & anaerobes | Reduced lactobacilli, increased pH, release of defensins | Weak specific antibody production; chronic inflammation | Thin gray discharge, fishy odor |
| Yeast Infection (Candida albicans) | Candida albicans | Elevated neutrophil influx, β‑defensin surge | Th17‑driven response, IgA antibodies in mucus | Itchy white cottage‑cheese discharge |
| Trichomoniasis | Trichomonas vaginalis | Macrophage activation, nitric oxide production | CD8+ T‑cell cytotoxicity, IgG antibodies | Yellow-green frothy discharge, irritation |
In BV the imbalance lets harmful bacteria overgrow, but the adaptive arm struggles to form lasting immunity, leading to recurrence. Candida elicits a robust Th17 response because fungi are hard to clear; insufficient IgA can let the infection linger. Trichomonas, a protozoan, provokes a strong cellular response, yet the parasite can evade detection by altering its surface proteins.
Factors That Weaken Vaginal Immunity
Even a well‑tuned immune system can be tipped off balance. Hormonal swings during the menstrual cycle or menopause reduce estrogen‑driven glycogen production, which feeds lactobacilli and lowers acidity. Antibiotics wipe out both harmful and beneficial bacteria, leaving a vacuum for opportunistic microbes.
Other culprits include uncontrolled diabetes (high glucose fuels yeast growth), chronic stress (cortisol suppresses cytokine production), and smoking (impairs ciliary clearance). Sexual activity with a new partner can introduce unfamiliar microbes, and lubricants with high glycerin content may feed Candida.
Boosting Your Vaginal Immune Defense
Most of the time you can reinforce your natural defenses without medication:
- Probiotic foods or supplements: Strains like Lactobacillusrhamnosus and Lactobacillusreuteri colonise the vagina and keep pH low.
- Balanced diet: Plenty of fiber, low‑sugar fruits, and fermented foods support a healthy microbiome.
- Smart hygiene: Avoid scented soaps, douches, and tight synthetic underwear that trap moisture.
- Safe sex practices: Use condoms, limit number of partners, and consider pre‑exposure prophylaxis for sexually transmitted infections that can disturb flora.
- Regular medical check‑ups: Screening for diabetes, hormonal imbalances, or recurrent infections can reveal underlying issues.
When infections do occur, early treatment limits inflammation and prevents long‑term changes to the immune landscape. For recurrent yeast infections, a short course of antifungal medication combined with a probiotic regimen often restores balance faster than drugs alone.

When to Seek Professional Care
If you notice persistent itching, unusual discharge, foul odor, or pain during intercourse that lasts more than a few days, it’s time to consult a healthcare provider. Repeated episodes (three or more per year) suggest an underlying immunity problem that may need targeted therapy such as hormonal treatment, bacterial vaginosis eradication protocols, or immune‑modulating medications.
Doctors may order a wet prep, culture, or PCR test to identify the exact pathogen and tailor treatment. In rare cases, chronic inflammation can lead to complications like pelvic inflammatory disease, so early intervention is crucial.
Frequently Asked Questions
Why do I get yeast infections more often after taking antibiotics?
Antibiotics kill both harmful bacteria and the beneficial Lactobacillus species that keep vaginal pH low. With fewer lactobacilli, Candida can grow unchecked, leading to infection.
Can the immune system completely prevent bacterial vaginosis?
BV is often linked to an imbalance rather than a single pathogen. The innate immune system can limit overgrowth, but without a strong adaptive response, recurrence is common. Restoring lactobacilli is key.
Do probiotics really work for preventing vaginal infections?
Clinical studies show that specific strains-especially Lactobacilluscrispatus and Lactobacillusjensenii-can reduce recurrence of BV and yeast infections by re‑establishing an acidic environment.
How does menopause affect vaginal immunity?
Lower estrogen reduces glycogen in vaginal cells, limiting food for lactobacilli. The resulting higher pH weakens the barrier, making infections more likely. Local estrogen therapy can restore the microbiome.
Is it safe to use over‑the‑counter antifungal creams repeatedly?
Occasional use is fine, but frequent self‑treatment can mask underlying issues and promote resistant strains. If you need treatment more than twice a year, see a clinician for a full work‑up.
14 Responses
Yo, the body’s own microbiome is basically the MVP of vaginal health – keep that acid vibe tight and the immune squad will shut down any unwelcome guests fast.
Indeed, the interplay between lactobacilli‑derived lactic acid and the innate immune arsenal creates a symphony of protection. When that balance tips, the cascade of cytokines can feel like an internal alarm system. I’ve seen patients describe the sudden onset of itching as “a fire alarm going off in the night.” Understanding these mechanisms helps us demystify that distress.
Cool science, but let’s not forget that over‑the‑counter creams aren’t magic wands. You slap a cream on, and if you keep the underlying dysbiosis, you’ll be back in the same spot in a week. So yeah, maybe think about a probiotic plan too.
From a microbiological standpoint, the colonization resistance conferred by Lactobacillus crispatus involves competition for glycogen-derived substrates and production of hydrogen peroxide, which jointly suppresses anaerobic overgrowth. This dynamic equilibrium is what keeps bacterial vaginosis at bay in most healthy individuals.
Keeping things simple: eat your veggies, stay away from scented soaps, and maybe add a daily probiotic yogurt. Your vagina will thank you.
Big pharma doesn’t want you to know natural immunity does most of the work.
In many cultures, women have been using fermented foods for centuries to keep the down‑there area balanced – it’s like a traditional prebiotic for the vag.
When we think about immunity, we often picture white blood cells marching like soldiers, but the vaginal environment adds a unique twist to that picture. The epithelial lining is not just a wall; it constantly sheds and renews, presenting fresh receptors for beneficial microbes. Lactobacilli thrive on the glycogen that estrogen‑stimulated cells release, turning it into lactic acid that keeps the pH low. This acidity isn’t just a number on a lab report – it creates a hostile arena for many pathogens. At the same time, pattern‑recognition receptors on the surface cells listen for trouble, ready to release defensins the moment something out of place appears. Neutrophils, often the first responders in blood, also patrol the mucosal surface and can gobble up invaders within minutes. Macrophages act like the neighborhood watch, cleaning up debris and presenting antigens to the adaptive arm. The T‑cell response, especially Th17 cells, is crucial when fungi try to set up shop, because they recruit more neutrophils and stimulate IgA production. Speaking of IgA, it coats the mucus, acting like a slippery shield that prevents microbes from attaching. Cytokines such as IL‑1β and TNF‑α serve as the alarm bells, increasing blood flow and bringing more immune cells to the front lines. Hormonal fluctuations during the menstrual cycle can tilt this balance; for example, lower estrogen in the luteal phase can reduce glycogen, slightly raising pH. That is why some women notice a higher susceptibility to yeast infections right before their period. Stress, through cortisol, can dampen cytokine production, loosening the coordinated defense. Even lifestyle factors like smoking introduce toxins that impair ciliary clearance, making the vagina more vulnerable. The bottom line is that immunity here is a collaborative dance between microbes, hormones, and immune cells, and keeping any one partner healthy supports the whole system. So regular check‑ups and mindful habits are the best way to keep this choreography in sync.
Your comprehensive overview elegantly captures the multifaceted interplay-yet it also invites a deeper contemplation of how sociocultural practices influence these biological processes, especially when dietary habits rooted in tradition either bolster or undermine the lactobacilli reservoirs; for instance, the regular consumption of fermented foods such as kefir or kimchi not only supplies exogenous probiotic strains but also modulates systemic immunity through gut‑vaginal axis signaling pathways. Moreover, the timing of probiotic intake relative to menstrual phases could theoretically synchronize with peak glycogen availability, optimizing colonization efficiency-a hypothesis that warrants rigorous longitudinal studies. It is also noteworthy that stress‑induced cortisol elevations, while often dismissed as merely “psychological,” have measurable effects on cytokine transcriptional activity, thereby subtly reshaping the vaginal microenvironment. By integrating these psychosocial variables with the molecular mechanisms you described, clinicians could adopt a more holistic treatment algorithm, one that personalizes interventions beyond the one‑size‑fits‑all prescription model.
Yo, great info! Just a heads up-watch out for “yeast” over‑thinking, u don’t need to freak out every time u feel a little itch. A quick probiotic shake can save u a whole lotta hassle.
One might ponder the existential significance of microbial symbiosis - is the vaginal flora not a microcosm of the larger universe, where every bacterial cell plays a role akin to a star in a galaxy, each emitting biochemical light that guides the immune nebula through darkness? When antibiotics disturb this delicate constellation, it is as if a supernova has exploded, scattering essential particles and leaving a void that opportunistic pathogens eagerly fill. Thus, the very act of taking a pill becomes a philosophical statement about humanity’s desire to dominate nature, often at the cost of our own internal ecosystems.
Don’t forget that staying hydrated and eating plenty of fiber can naturally support the good bacteria. It’s amazing how small daily habits can create big protective effects for your intimate health.
The truth is, the “big pharma” narrative keeps us from learning that simple diet tweaks are actually the most powerful weapon against infections – it’s a silent war they don’t want you to see.
All in all, balancing lifestyle, mindful hygiene, and occasional medical guidance seems like the smartest route for long‑term vaginal wellness.