Vaginal Microbiome – What It Is and Why It Matters
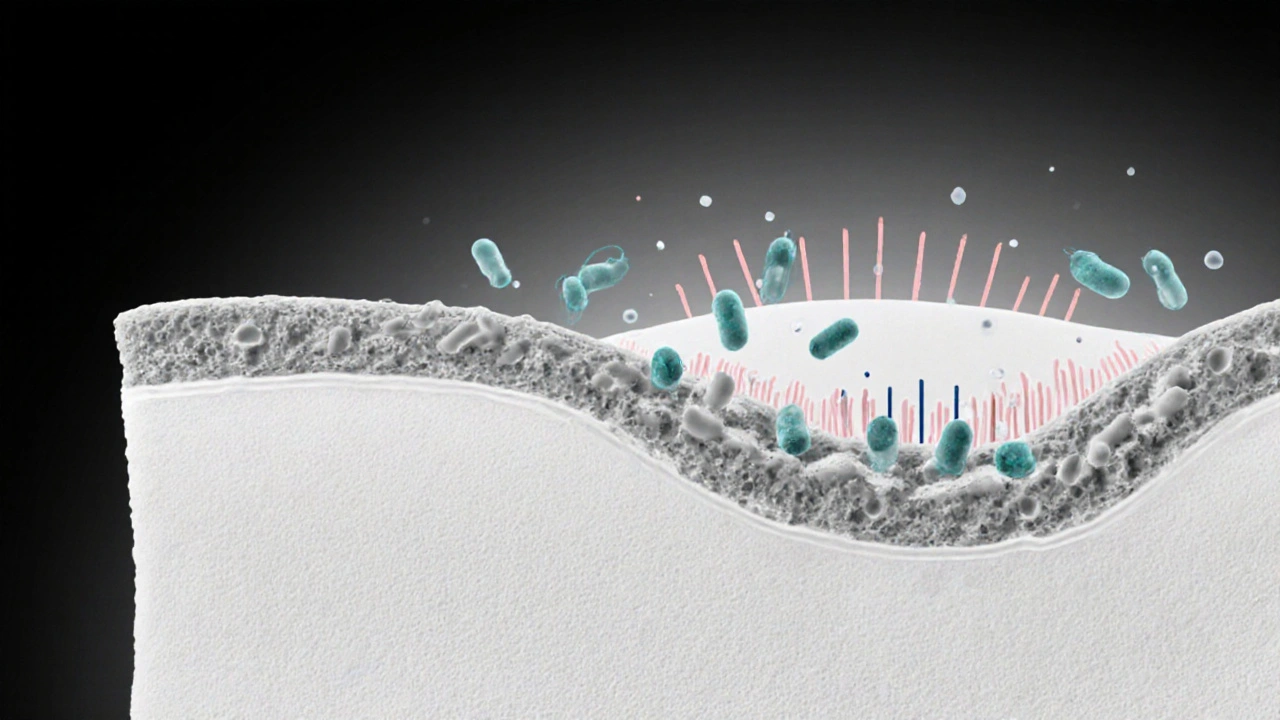
When you hear about vaginal microbiome, the community of bacteria living in the vagina that helps keep the area balanced and protects against infections. Also known as vaginal flora, it plays a central role in women's reproductive health. Understanding this ecosystem lets you see how hormones, medications, and life stages shape what’s happening down there.
Lactobacillus the dominant good bacteria that produce lactic acid and keep the vaginal pH low is the star player in a healthy vaginal microbiome. Menopause the natural decline in estrogen that occurs in later reproductive years often reduces Lactobacillus numbers, leading to higher pH and susceptibility to irritation. Hormonal contraception birth control methods that release estrogen or progestin can either support or disturb this balance, depending on the formulation. Meanwhile, Antibiotics drugs that kill bacteria, sometimes wiping out beneficial strains may unintentionally knock down Lactobacillus, setting the stage for yeast overgrowth or bacterial vaginosis. These connections illustrate why any change in hormones or medication can ripple through the vaginal ecosystem.
How Lifestyle and Health Choices Impact Your Vaginal Microbiome
Every month the menstrual cycle shakes up the bacterial mix. During the fertile phase estrogen rises, encouraging Lactobacillus growth, while the luteal phase sees a dip that can let opportunistic microbes sneak in. If you’re trying to conceive, a stable microbial environment supports sperm motility and implantation, which is why many fertility specialists ask about recent antibiotic courses or probiotic use.
Sexual activity also plays a part. New partners introduce foreign bacteria, and condom use can protect the resident community by reducing fluid exchange. Conversely, douching or harsh soaps strip away the natural mucus layer, making it harder for good bacteria to cling. Simple habits like wearing breathable underwear, avoiding scented products, and staying hydrated keep the pH in check and give Lactobacillus a fighting chance.
When an infection strikes, the body’s response can further shift the microbiome. Bacterial vaginosis, for example, is a classic case of reduced Lactobacillus and overgrowth of anaerobes. Treating it with metronidazole works, but the drug can also blunt the beneficial strains, so a follow‑up probiotic regimen is often recommended to re‑establish balance.
Probiotics marketed for vaginal health usually contain strains like Lactobacillus rhamnosus or L. crispatus. Clinical trials show they can lower recurrence of yeast infections and help maintain a low vaginal pH after antibiotics. However, not all products are created equal—look for clinically tested formulations and talk to a healthcare provider before starting any supplement.
All these factors—hormonal shifts, medication, hygiene, and sexual habits—interact in a dynamic web. By understanding how they influence the vaginal microbiome, you can make smarter choices that protect your comfort and reproductive goals. Below you’ll find articles that dive deeper into menopause, fertility options, medication safety, and more, all tied back to the health of this often‑overlooked ecosystem.
How the Immune System Prevents and Fights Vaginal Infections
- Laura Ledas
- Aug, 22 2025
Learn how the immune system protects the vagina, why infections happen, and practical steps to strengthen your natural defenses.
Learn More