Therapeutic Drug Monitoring: What It Is and Why It Matters for Your Medications
When you take a medicine like therapeutic drug monitoring, a clinical process that measures the amount of a drug in your bloodstream to ensure it’s working safely and effectively. Also known as TDM, it’s not just for hospital patients—it’s a quiet backbone of care for people on long-term meds like seizure drugs, heart medications, or antidepressants. If your dose is too low, the drug won’t help. Too high, and you risk serious side effects. TDM bridges that gap by using simple blood tests to find your personal sweet spot.
This isn’t guesswork. Doctors use drug levels, the measured concentration of a medication in your blood at a specific time to decide if your current dose needs tweaking. For example, someone on warfarin, a blood thinner that requires careful dosing to avoid clots or bleeding might get checked every few weeks. Same with lithium, a mood stabilizer with a narrow safety window—even a small change in your body’s absorption can push it into dangerous territory. That’s why TDM saves lives: it turns trial-and-error into precision medicine.
It’s not just about the drug itself. Your body changes. Age, liver function, other meds, even what you eat can shift how fast your system processes a drug. That’s why drug interactions, when one medication affects how another is absorbed, broken down, or cleared matter so much in TDM. A common antibiotic might slow down how quickly your body clears an antidepressant, causing levels to spike. Without monitoring, you’d never know why you suddenly felt dizzy or nauseous. And that’s exactly why posts here cover real cases—like tramadol risks tied to enzyme blockers, or how cinnarizine needs careful dosing in older adults. These aren’t abstract ideas. They’re daily realities for people managing chronic conditions.
What you’ll find below isn’t a textbook. It’s a collection of real-world stories and science-backed guides that show how TDM shows up in practice. From antihistamines that build up in seniors to blood thinners that demand constant tracking, each post ties back to one simple truth: knowing how much of a drug is in your body isn’t optional—it’s essential. Whether you’re on a daily pill, just started a new treatment, or help someone who is, this is the info that helps you ask the right questions—and stay safe while doing it.
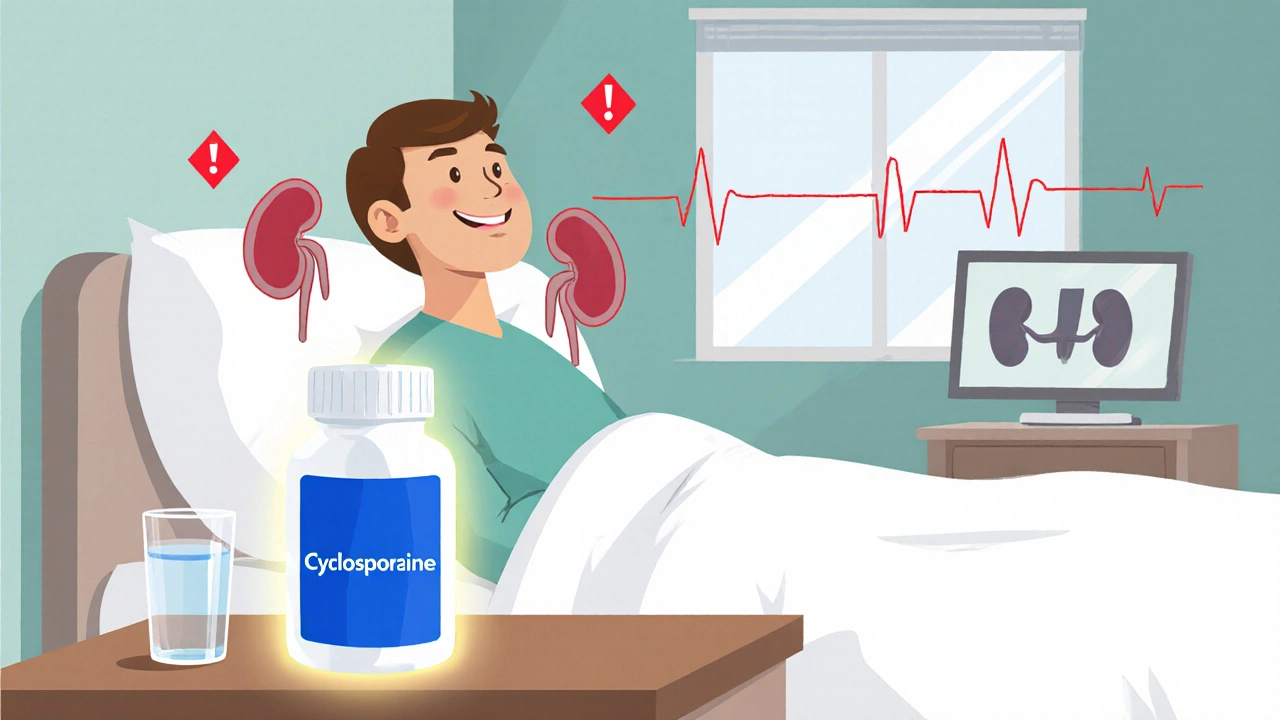
Cyclosporine Nephrotoxicity: How to Monitor Kidney Function & Drug Levels
- Laura Ledas
- Oct, 26 2025
Learn how to safely monitor cyclosporine levels and kidney function to avoid nephrotoxicity, with clear schedules, lab tips, and dose‑adjustment strategies.
Learn More