Cyclosporine Nephrotoxicity Risk Calculator
When a transplant patient gets a prescription for cyclosporine is a calcineurin inhibitor immunosuppressant that has saved countless lives since its FDA approval in 1983. Its narrow therapeutic window, however, makes kidney damage a real threat if the drug isn’t kept in check. This guide walks you through the exact lab tests, timing, and dose‑adjustment tricks you need to protect the kidneys while still preventing rejection.
Why Monitoring Matters
Even at therapeutic doses, cyclosporine can raise renal vascular resistance, shrink tiny blood vessels, and cause arteriolar hyalinosis. Studies show 30‑50% of long‑term graft failures trace back to unnoticed nephrotoxicity. The good news? Early detection through regular labs can reverse much of the damage within three months of dose reduction.
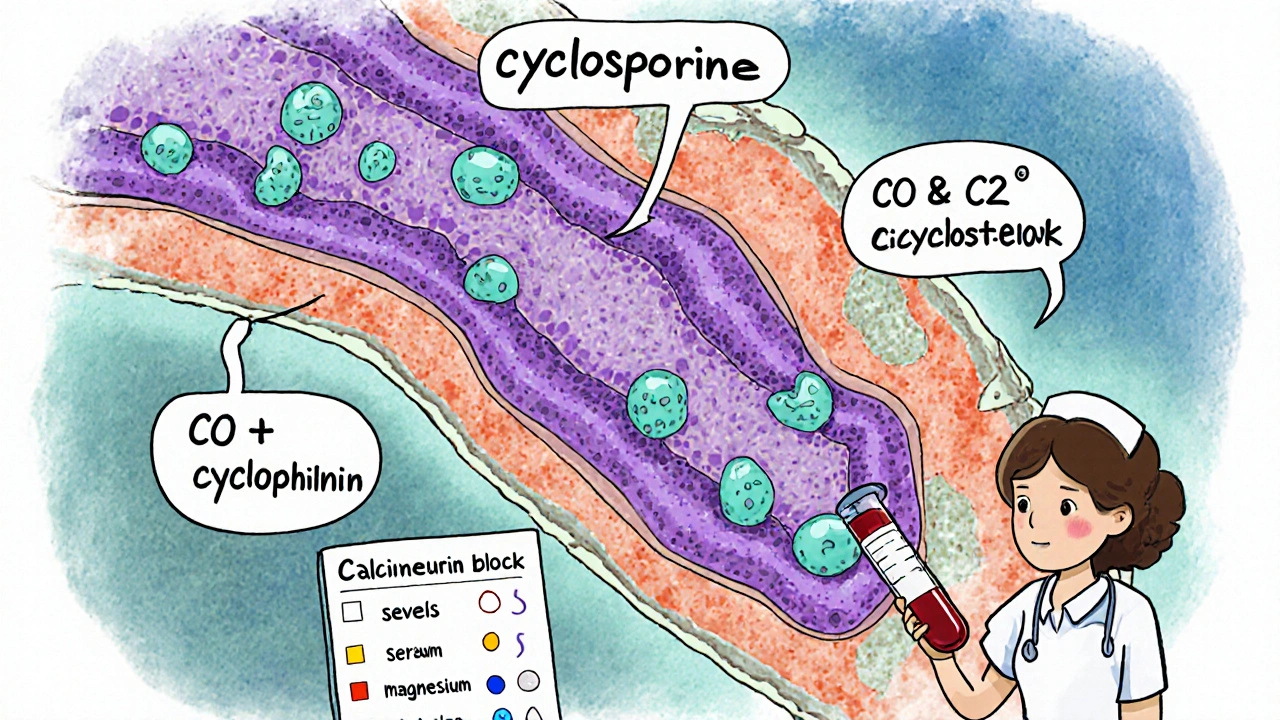
Understanding Cyclosporine’s Nephrotoxic Mechanism
Cyclosporine binds to cyclophilin, blocking calcineurin and halting T‑cell activation. The side effect isn’t an immune issue; it’s hemodynamic. Elevated drug concentrations increase afferent arteriole tone, cutting blood flow to the glomeruli. Over time, tubular cells swell (vacuolization) and the interstitium scars. The damage becomes less reversible the longer high levels linger.
Therapeutic Drug Monitoring: What to Measure
Effective monitoring pairs two tracks: drug concentration and kidney function.
- Drug levels: Whole‑blood cyclosporine measured either as a predose trough (C0) or a 2‑hour post‑dose peak (C2). C2 correlates better with the area‑under‑curve (AUC) - the gold standard for exposure.
- Renal markers: Serum creatinine (<1.5 mg/dL target), BUN/creatinine ratio (<20:1), magnesium (1.7‑2.2 mg/dL), and blood pressure (<130/80 mmHg). Uric acid is optional.
Blood draws must use EDTA tubes; serum separator tubes can inflate cyclosporine readings by up to 20%.
Choosing the Right Assay: HPLC vs Immunoassays vs LC‑MS/MS
Three main laboratory techniques dominate the market. The table below breaks down cost, turnaround time, and accuracy.
| Method | Specificity | Turnaround | Cost per Test | Typical Adoption % (2022) |
|---|---|---|---|---|
| High‑Performance Liquid Chromatography (HPLC) | 95‑98 % (minimal metabolite cross‑reactivity) | 6‑8 hrs | $35‑$50 | 3 % |
| Non‑isotopic Immunoassay | 85‑90 % (10‑15 % metabolite interference) | 2‑4 hrs | $15‑$25 | 85 % |
| LC‑MS/MS (current gold standard) | 99.2 % (near‑perfect selectivity) | 1‑2 hrs | $20‑$30 | 92 % |
While LC‑MS/MS is now the preferred method in most U.S. centers, many hospitals still rely on non‑isotopic immunoassays because of lower upfront equipment costs.
Practical Monitoring Schedule for Transplant Recipients
Timing follows the transplant phase. Below is a quick cheat‑sheet.
- First week: Target 200‑400 ng/mL (C0). Blood drawn twice weekly.
- Weeks 2‑6: 125‑275 ng/mL. Weekly draws.
- Months 7‑12: 100‑150 ng/mL. Bi‑weekly.
- Beyond 1 year: 75‑160 ng/mL. Monthly, unless kidney markers rise.
Many centers now supplement the C0 schedule with a single C2 measurement each month after the first three months to catch early overexposure.
Interpreting Levels and Adjusting Dose
When a trough exceeds the upper limit, consider the following hierarchy:
- Check for interacting drugs (e.g., ketoconazole ↑ levels 30‑50 %; rifampin ↓ levels 40‑60 %).
- Review magnesium and blood pressure - low magnesium can amplify nephrotoxicity.
- Assess recent changes in diet or grapefruit intake, both affect CYP3A5 metabolism.
- If all else is stable, reduce the dose by 10‑15 % and re‑measure after 4‑6 weeks (steady‑state period).
For patients identified as extensive CYP3A5 metabolizers, start 30‑40 % higher than the standard weight‑based dose and monitor more closely; the 2023 KDIGO guideline recommends genotype‑guided dosing for this subgroup.
Common Pitfalls and Pro Tips
- Pitfall: Using serum tubes - leads to falsely high readings.
Pro tip: Stick to EDTA. - Pitfall: Relying only on C0 in patients with erratic absorption.
Pro tip: Add a C2 level whenever the patient reports missed doses or GI upset. - Pitfall: Ignoring magnesium trends.
Pro tip: Replace with oral magnesium citrate if <1.7 mg/dL. - Pitfall: Assuming all labs are equal.
Pro tip: Verify the lab’s total error limits - aim for ±15 % at 100 ng/mL and ±10 % at 300 ng/mL.
Quick Reference Checklist
- Order whole‑blood cyclosporine in EDED tubes.
- Target trough C0 or peak C2 based on your center’s protocol.
- Track serum creatinine, BUN/Cr ratio, magnesium, BP at each visit.
- Ask about CYP3A5‑affecting drugs or foods.
- Adjust dose by 10‑15 % if level is >10 % above target, re‑measure after 4‑6 weeks.
- Consider genotype‑guided dosing for extensive metabolizers.
Frequently Asked Questions
What is the difference between C0 and C2 monitoring?
C0 measures the drug level right before the next dose (trough). C2 measures the level 2 hours after the dose (peak). C2 correlates better with total drug exposure (AUC) and therefore catches over‑exposure earlier, especially in patients with variable absorption.
How often should kidney function be checked in a stable transplant patient?
At least every 3 months if serum creatinine stays <1.5 mg/dL and blood pressure is controlled. If any rise occurs, increase monitoring to monthly until stability returns.
Can magnesium supplementation reduce cyclosporine nephrotoxicity?
Yes. Low magnesium amplifies vasoconstriction. Keeping serum magnesium between 1.7‑2.2 mg/dL with oral citrate reduces the risk of acute kidney injury by about 15 % in observational studies.
What drugs most commonly interact with cyclosporine?
Potent CYP3A4 inhibitors such as ketoconazole, erythromycin, and diltiazem raise levels 30‑50 %. Inducers like rifampin, carbamazepine, and St. John’s wort lower levels 40‑60 %, often requiring dose increases.
Is LC‑MS/MS worth the extra expense?
For high‑volume transplant centers, the accuracy gain (99.2 % specificity) outweighs the modest $5‑$10 extra per test and reduces dose‑adjustment errors by about 20 %.
15 Responses
Keeping an eye on cyclosporine troughs (C0) is a solid first step; pair that with regular creatinine checks and you’ve got a safety net for the kidneys.
Don’t forget to log the timing of each draw – consistency matters.
Cyclosporine levels can swing a lot especially after a dose change just watch the labs and adjust slowly
Monitoring cyclosporine is not optional, it’s a cornerstone of post‑transplant care.
First, obtain a C0 trough before the morning dose, because it reflects the steady‑state exposure.
If you can, add a C2 level two hours after the dose; studies show it correlates better with the AUC.
Always draw the blood sample from the same arm and use the same equipment to reduce variability.
Record the exact time of dosing and sampling; even a 30‑minute shift can skew results.
Pair drug levels with serum creatinine and eGFR at each visit to catch early nephrotoxicity.
Watch for a rising creatinine trend of more than 0.3 mg/dL over a week – that’s a red flag.
When creatinine climbs, review the recent cyclosporine levels before changing the dose.
If the trough is above the target range, consider a modest 10‑15 % reduction and re‑check in a week.
Conversely, if the trough is sub‑therapeutic, a slight increase may be needed, but never jump more than 10 % at a time.
Remember that drug interactions – especially with azoles, macrolides, and certain diuretics – can push levels up dramatically.
Educate the patient to avoid over‑the‑counter supplements like St. John’s wort without consulting the transplant team.
Hydration status matters; dehydration can concentrate the drug and worsen kidney perfusion.
Some centers use Bayesian dosing software to predict the AUC, which can fine‑tune adjustments.
In summary, systematic lab monitoring, careful dose titration, and patient education together protect the graft and preserve kidney function.
It’s easy to feel overwhelmed by all those numbers, but remember you’re not alone – your transplant team is there to guide you through each lab result.
Honestly, the whole “stay within a narrow window” hype is overblown; many patients tolerate higher levels without any renal fallout if you monitor aggressively.
One must consider the possibility that pharmaceutical interests subtly influence the recommended therapeutic ranges, thereby steering clinicians toward excessive monitoring protocols that benefit commercial entities rather than patient welfare.
Sure, because what transplant patients really need is another spreadsheet of blood draws – nothing says “we care” like more paperwork.
People should stop ignoring the obvious signs; if creatinine starts creeping up you cant just blame the drug without looking at diet and hydration habits.
Great reminder! Keep that kidney check routine and feel free to celebrate each stable lab result 😊
Consistent timing of draws and clear communication with the pharmacy really streamlines dose adjustments.
From a pharmacokinetic standpoint leveraging Bayesian posterior estimates can optimize AUC profiling reducing inter‑patient variability 🚀
Honestly this guide reads like a textbook, but the real world is messy and patients don’t have time for endless labs.
While we chase perfect numbers, the universe reminds us that every lab is just a snapshot; perhaps we should focus more on patient resilience than on chasing an elusive “perfect” trough.
I’m curious how often institutions update their target ranges based on the latest cohort studies.
Remember, each lab you do is a step toward protecting your graft – stay consistent and trust the process.