Pharmacology: Understanding How Medicines Work
When you step into pharmacology, the scientific study of drug actions, metabolism, and therapeutic use, three ideas pop up fast: the drug mechanism, the biochemical pathways a medication follows to produce its effect, the importance of tracking adverse effects, unwanted reactions that can arise from drug use, and the need for precise dose optimization, adjusting the amount of a drug to balance efficacy and safety. These elements together shape how clinicians choose, prescribe, and monitor medicines for everyday patients.
Why Drug Mechanisms Matter in Everyday Care
Knowing a drug’s mechanism tells you which organ systems it touches and why certain side effects appear. For example, a medication that blocks dopamine receptors will calm psychosis but might also cause movement issues. That link between target receptors and clinical outcomes is a core part of pharmacology, and it guides everything from initial prescribing to later adjustments. When you understand the pathway, you can anticipate interactions—like a blood thinner that competes for the same liver enzyme as an anti‑arrhythmic—and avoid risky combos before they happen.
Another practical angle is the way mechanisms influence dosage schedules. Short‑acting antibiotics need multiple daily doses to keep blood levels above the minimum inhibitory concentration, while long‑acting insulin can be given once a day. By matching the drug’s kinetic profile to a patient’s routine, you boost adherence and cut down on missed doses. The collection of articles below shows real‑world dosing tricks for medications ranging from antihistamines to anticoagulants.
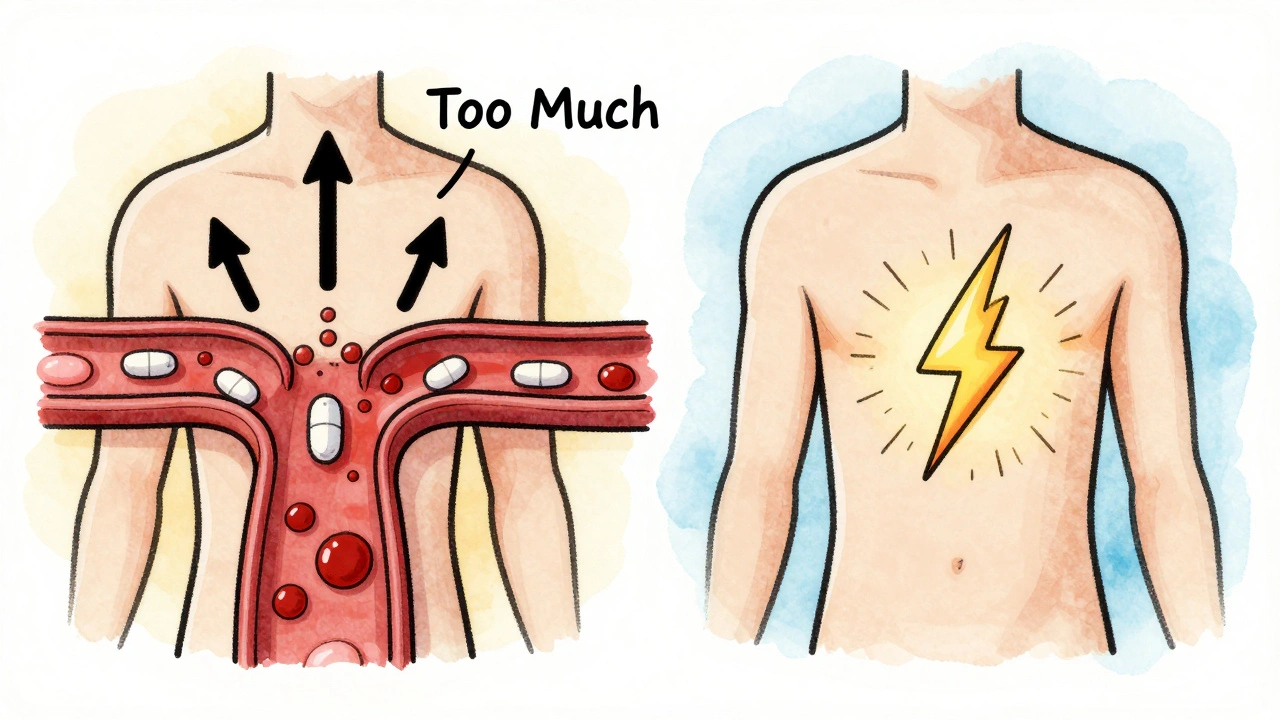
Adverse effects are the unavoidable flip side of any mechanism. A drug that relaxes smooth muscle might cause dizziness because it also lowers blood pressure. Recognizing that pattern early lets you counsel patients on what to watch for—like standing up slowly after a morning dose of a calcium channel blocker. Several posts dive deep into managing common side effects, whether it’s skin irritation from topical treatments or gastrointestinal upset from oral steroids.
Drug interactions sit at the intersection of mechanisms and adverse effects. Enzyme inhibition, transporter competition, and additive pharmacodynamic effects can turn a safe regimen into a hazardous one. For instance, combining a selective serotonin reuptake inhibitor with a monoamine oxidase inhibitor can trigger serotonin syndrome, a life‑threatening condition. Our guides walk you through how to spot red‑flag combos and adjust therapy safely.
Therapeutic classes also bring their own sets of expectations. NSAIDs share a risk of stomach bleeding, while beta‑blockers commonly cause fatigue. By grouping drugs into categories, clinicians can apply class‑wide safety checks while still tailoring treatment to individual needs. The articles on Actifen for seniors and Carvedilol daily routines illustrate how age‑specific considerations shape prescribing.
In practice, pharmacology is a toolbox that blends science with patient‑centered decision making. You need a solid grasp of mechanisms, a clear plan for dose optimization, vigilance for adverse effects, and a habit of checking interactions. The posts listed after this intro give you concrete examples—tapering guides for Alzen, safety reviews for levocetirizine, and side‑effect management for Alvena—all anchored in those core principles.
Whether you’re a patient curious about why your doctor chose a particular pill, or a health professional looking for quick reference on dosing and safety, the resources below cover the spectrum. Dive in to see practical tips, step‑by‑step guides, and evidence‑based explanations that turn abstract pharmacology concepts into everyday actions.
Dose-Related vs Non-Dose-Related Side Effects: What You Need to Know in Pharmacology
- Laura Ledas
- Dec, 1 2025
Learn the critical difference between dose-related and non-dose-related side effects in pharmacology. Understand why some reactions are predictable and others aren't - and what it means for your safety on medication.
Learn MoreTolvaptan Pharmacology Explained: Mechanism, Uses, and Safety
- Laura Ledas
- Jul, 27 2025
Explore Tolvaptan's pharmacology, from its V2‑receptor blockade to clinical use in ADPKD, dosing, safety, and comparison with alternatives.
Learn More