Side Effect Type Checker
Understand Your Side Effect
This tool uses principles from the article to help you determine if your side effect is likely dose-related or non-dose-related. Your input helps estimate whether it's related to the amount of medication you're taking or an unpredictable reaction.
When you take a pill, your body reacts. Sometimes, that reaction is helpful. Other times, it’s not. That’s where side effects come in. But not all side effects are the same. Some happen because you took too much. Others happen for reasons you can’t predict - even if you took the exact right dose. Understanding the difference between dose-related and non-dose-related side effects isn’t just for doctors. It’s crucial for anyone taking medication regularly.
What Are Dose-Related Side Effects?
Dose-related side effects - also called Type A reactions - are predictable. They happen because the drug is doing exactly what it’s supposed to do, just too well. Think of them as an extension of the drug’s main effect, turned up too loud.
Take blood pressure meds. If your doctor prescribes a drug to lower your systolic pressure from 160 to 130, but it drops to 90, you might feel dizzy, faint, or even pass out. That’s not a new problem - it’s the same effect, just stronger. Same with insulin: too much, and your blood sugar crashes below 70 mg/dL. That’s hypoglycemia - a classic dose-related reaction.
These reactions follow the law of mass action: more drug in your system = more effect. That’s why they’re so common. About 70 to 80% of all adverse drug reactions fall into this category. And they’re especially dangerous with drugs that have a narrow therapeutic window - meaning the difference between the right dose and the toxic dose is tiny.
Drugs like digoxin (for heart failure), lithium (for bipolar disorder), and warfarin (a blood thinner) are notorious for this. Digoxin’s safe range? 0.5 to 0.9 ng/mL. Over 2.0? You’re in toxic territory. Lithium’s safe level? 0.6 to 1.0 mmol/L. Go above 1.2? You risk seizures or kidney damage.
Why do these happen so often in older adults? Because aging slows how your body clears drugs. Your kidneys and liver don’t work as fast. A dose that was fine at 40 might be dangerous at 70. Add in other medications - like antibiotics that block how your liver breaks down statins - and the risk multiplies. A 2011 study found that over two-thirds of emergency visits for drug reactions in people over 65 were caused by anticoagulants, insulin, and diabetes pills - all classic dose-related offenders.
What Are Non-Dose-Related Side Effects?
Non-dose-related side effects - Type B reactions - are the opposite. They’re unpredictable. They don’t make sense based on how the drug works. And they can happen even with the smallest dose.
Imagine taking one pill of amoxicillin and breaking out in a full-body rash, blisters, and peeling skin. That’s Stevens-Johnson syndrome - a rare but deadly Type B reaction. Or you take penicillin and suddenly can’t breathe, your throat swells, your blood pressure crashes. That’s anaphylaxis. Neither of these has anything to do with how much you took. They’re about your body’s immune system going rogue.
These reactions are rare - only 15 to 20% of all adverse reactions - but they’re responsible for 70 to 80% of serious drug-related hospitalizations and deaths. That’s because they’re often severe, sudden, and hard to treat. Once they happen, the drug must be stopped forever. No dose adjustment. No waiting it out. You can’t take it again.
Some Type B reactions need prior exposure. Like a first-time allergy to penicillin - it usually doesn’t happen on the first dose. But after one exposure, your immune system remembers. Next time, even a tiny amount triggers a massive reaction. Others, like certain skin rashes from lamotrigine or carbamazepine, can strike on the first dose, no warning.
Genetics play a huge role. For example, if you carry the HLA-B*57:01 gene, taking abacavir (an HIV drug) gives you a 50% chance of a life-threatening allergic reaction. Test for the gene first? That risk drops to near zero. That’s why genetic screening is now standard before prescribing abacavir in many countries. The test costs around $150 to $300 - a small price to avoid a hospital stay.
Why the Confusion? The Dose Paradox
You might wonder: if all drugs act on the body through chemical reactions, how can any reaction truly be non-dose-related? Shouldn’t more drug always mean more effect?
That’s the paradox. And it’s been solved. Experts like Dr. Jeffrey Aronson explain that Type B reactions aren’t truly dose-free - they just have thresholds so low or so variable that they appear that way in most people.
Imagine a group of 1,000 people taking the same drug. For 990, the drug causes no reaction until they hit 100 mg. But for 10, even 1 mg triggers a violent immune response. In population studies, you’d see these 10 people having reactions at low doses - while the rest need high doses. The reaction looks random. But it’s not. It’s about individual biology.
Other reasons include: measurement errors (did the patient really take the dose?), mistaken diagnosis (was it really the drug?), or hypersusceptibility - where the body hits its maximum reaction at a dose so low, increasing it doesn’t make things worse.

How Doctors Handle Each Type
Managing these two types of reactions is completely different.
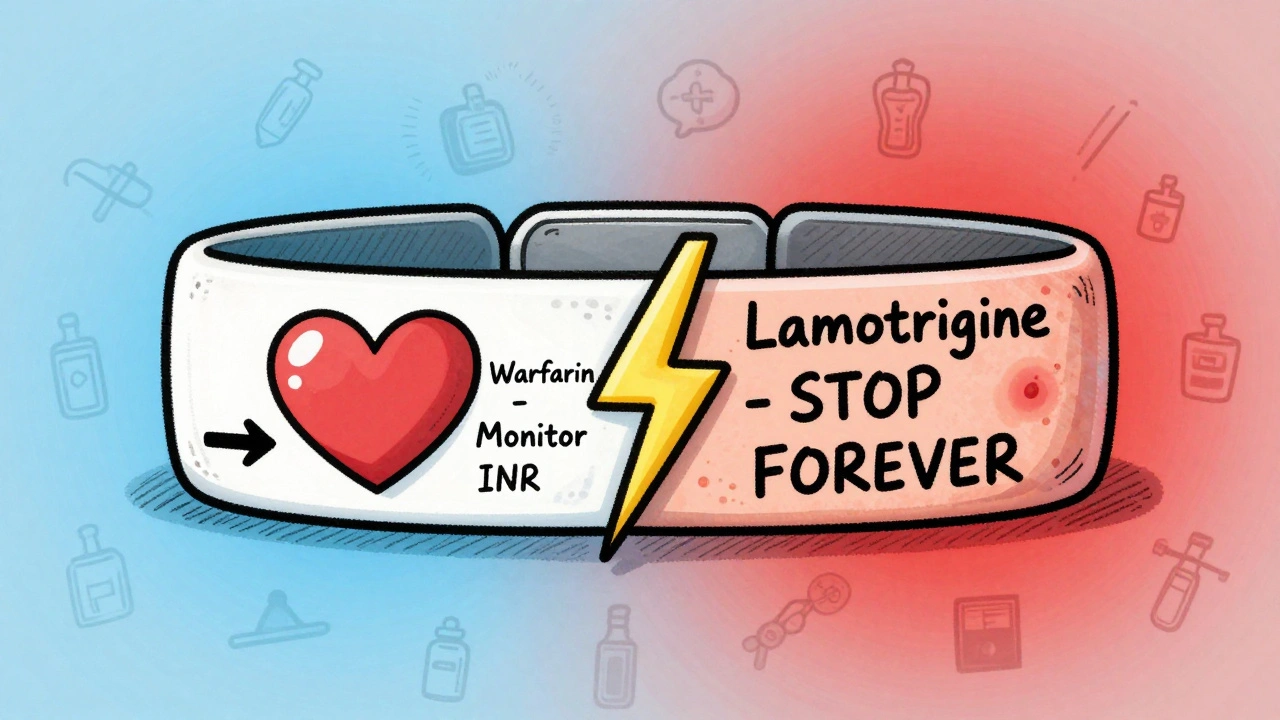
For dose-related (Type A) reactions, the fix is usually simple: lower the dose. Or monitor more closely. That’s why doctors check blood levels of drugs like vancomycin, phenytoin, and digoxin. They know the safe range. If levels creep too high, they adjust. They also watch for drug interactions. If you’re on warfarin and start taking amiodarone, your blood thinner levels can spike - so your INR gets checked more often.
For non-dose-related (Type B) reactions, there’s no adjusting. No monitoring. No safe dose. The only answer is stopping the drug - permanently. And avoiding similar drugs. If you had a severe reaction to penicillin, you likely can’t take amoxicillin, ampicillin, or other beta-lactams either.
Some Type B reactions can be screened for before they happen. HLA-B*15:02 testing before carbamazepine in Asian populations cuts the risk of Stevens-Johnson syndrome by 97%. Skin tests for penicillin allergy - while not perfect - can rule out true allergies in 90% of people who think they’re allergic.
Real-Life Examples
One doctor on Medscape described a patient whose INR shot to 8.2 after starting amiodarone - a classic Type A interaction. They adjusted the warfarin dose, monitored weekly, and kept the patient safe.
Another patient, on the same forum, developed Stevens-Johnson syndrome on her first dose of lamotrigine - even though she followed the slow titration schedule exactly. No warning. No dose error. Just her immune system flipping a switch. She now carries an epinephrine auto-injector.
On patient forums, people share stories like: “I took one 500mg amoxicillin pill. Within hours, my skin started peeling. My doctor said it wasn’t the dose - it was me.” These aren’t rare. They’re terrifying. And they’re Type B.
What’s Changing in Pharmacology?
The field is shifting toward personalization. Pharmacogenomics - using your genes to predict how you’ll react to drugs - is growing fast. The global market is projected to hit nearly $18 billion by 2030. The FDA now includes pharmacogenomic info on over 300 drug labels. For 28 drugs, genetic testing is required before prescribing.
Machine learning is helping too. Algorithms analyzing electronic health records can predict Type A reactions with 82% accuracy. But Type B? Only 63%. That’s because Type B reactions depend on complex immune responses, not just chemistry. They’re harder to see coming.
Regulators are catching up. The European Medicines Agency now distinguishes between “dose-independent” and “dose-unrelated” reactions. The NIH’s CPIC guidelines give doctors clear dosing rules for 53 gene-drug pairs - including both Type A (like warfarin and CYP2C9) and Type B (like abacavir and HLA-B).
What You Can Do
If you’re on long-term medication:
- Know your drugs. Ask your pharmacist: “Is this one of those that needs blood tests?”
- Report any new rash, fever, swelling, or breathing trouble - even if you think it’s minor. Don’t wait.
- Keep a list of all medications and supplements. Drug interactions are a leading cause of Type A reactions.
- If you’ve had a severe reaction, carry a medical alert card or bracelet. Say exactly what drug caused it.
- Ask about genetic testing if you’re prescribed drugs like abacavir, carbamazepine, or thiopurines.
Most side effects are dose-related. They’re manageable. But the ones that aren’t? They’re the ones that change your life. Knowing the difference could save it.
Are all side effects caused by taking too much medication?
No. While many side effects happen because the dose is too high - these are called dose-related or Type A reactions - others happen regardless of dose. These are non-dose-related or Type B reactions, often caused by your immune system reacting unexpectedly to the drug. You could take the correct dose and still have a severe reaction.
Can a non-dose-related reaction happen on the first dose of a drug?
Yes. While some immune reactions like penicillin allergy need prior exposure, others - such as Stevens-Johnson syndrome from lamotrigine or carbamazepine - can occur after the very first dose. There’s no warning, and it’s not because you took too much. It’s because your body reacted in a way that’s unique to you.
Why are Type B reactions more dangerous than Type A?
Type B reactions are less common but far more severe. While Type A reactions like low blood pressure or low blood sugar can be fixed by adjusting the dose, Type B reactions - like anaphylaxis or toxic skin reactions - can be fatal. They often require emergency treatment, hospitalization, and permanent avoidance of the drug. About 70-80% of serious drug-related hospitalizations are due to Type B reactions.
Is there a way to prevent non-dose-related side effects?
Yes, for some. Genetic testing can prevent serious reactions in high-risk people. For example, testing for the HLA-B*57:01 gene before taking abacavir prevents life-threatening allergies in nearly everyone who carries it. Skin tests can help rule out true penicillin allergies. But for many Type B reactions, there’s still no way to predict who will react - making early reporting of symptoms critical.
Do older adults get more dose-related side effects?
Yes. As we age, our kidneys and liver process drugs more slowly. This means drugs stay in the body longer, increasing the risk of buildup and overdose - even at normal doses. That’s why older adults are more likely to have hospital visits due to Type A reactions from blood thinners, diabetes meds, and heart drugs. Doctors often start them on lower doses and monitor more closely.
Can a drug have both types of side effects?
Absolutely. Many drugs cause both. For example, amoxicillin can cause diarrhea (a dose-related effect from killing gut bacteria) and a severe rash (a non-dose-related immune reaction). One is predictable and manageable. The other is sudden, dangerous, and permanent. That’s why it’s important to report every new symptom - not just assume it’s normal.
13 Responses
This is such a clear breakdown! I’ve had a friend go through Stevens-Johnson after one dose of lamotrigine - no warning, no mistake. Just pure bad luck. Glad this post highlights how it’s not about dosage. 😊
The distinction between Type A and Type B reactions is critical, yet rarely explained with such precision. I appreciate the inclusion of pharmacogenomic data and the emphasis on genetic screening for abacavir. This is textbook-level clarity.
In India, we’ve known this for decades. Our Ayurvedic systems always warned against indiscriminate drug use. Modern Western medicine is only now catching up. The fact that you need genetic testing for abacavir? That’s laughable. We’ve been avoiding toxic reactions with herbal detox protocols for centuries.
Dose-related side effects? Yeah, that’s just your body screaming, ‘Hey, chill with the pills!’ But non-dose-related? That’s your immune system throwing a full-on rave party with zero invitation. One minute you’re fine, next minute your skin’s peeling like a bad sunburn. No warning. No mercy. Just pure biological betrayal.
The real problem isn't the drugs it's the system that lets people self-diagnose and then demand prescriptions without any oversight. Type B reactions are just the tip of the iceberg. The real killer is the pharmaceutical industry pushing drugs without proper long-term data and doctors too lazy to monitor properly
They say Type B reactions are random but I’ve seen the pattern. All the people who had severe reactions? They all ate GMOs, took fluoride toothpaste, and lived near cell towers. The drug didn’t cause it - the environment did. The FDA knows this. They just won’t admit it because Big Pharma owns them.
So let me get this straight - you’re telling me that if I take one pill and my body turns on me, it’s not because I took too much… it’s because I’m just somehow broken? Like, I’m the glitch in the matrix? Cool. So what’s the fix? Don’t take medicine? Or just hope I don’t get sick?
You mention ‘70–80% of serious hospitalizations’ are due to Type B reactions... but you don’t mention the fact that most of those patients were on 5+ medications simultaneously. You’re blaming the drug, but the real issue is polypharmacy - and the medical system’s obsession with treating symptoms instead of root causes. This is a Band-Aid on a hemorrhage.
If you’re on long-term meds, please - please - talk to your pharmacist. They’re the unsung heroes of medication safety. I once had a patient come in with a rash after starting a new antibiotic. Turns out, it interacted with her herbal tea. She didn’t even think it counted as a ‘drug.’ We caught it before it got worse. Knowledge saves lives.
The data is sound. The structure is logical. The conclusion is valid. No further commentary required.
I’m so proud of how far we’ve come - genetic testing before prescribing? YES! Early detection? YES! Patient education? ABSOLUTELY! This is the kind of medicine we should be proud of - science, compassion, and personalization all working together. Keep sharing this. It matters. 💪❤️
I took lithium for a year. Never had an issue. Then one day I felt off. Turned out my thyroid meds were slowing my clearance. My dose was fine. My body just changed. This post nailed it. Dose-related isn’t always about the pill. It’s about you.
To anyone reading this who’s scared of meds - you’re not alone. I used to avoid every new prescription because I was terrified of a reaction. But learning the difference between ‘my body’s too sensitive’ and ‘I took too much’ changed everything. It didn’t make me less anxious, but it made me feel less powerless. You’re not broken. You’re just unique. And that’s okay.