Kidney Transplant: What You Need to Know About Recovery, Medications, and Long-Term Care
When your kidneys can't keep up, a kidney transplant, a surgical procedure where a healthy kidney from a donor replaces a failing one. Also known as renal transplant, it's often the best long-term solution for end-stage kidney disease, offering more freedom than dialysis and better quality of life for most people. Unlike dialysis, which filters your blood mechanically, a transplanted kidney works naturally—regulating fluids, removing waste, and helping control blood pressure. But getting a new kidney isn't the end of the story. It's the start of a new routine built around medications, checkups, and watching for signs your body might be rejecting it.
After the surgery, you'll take immunosuppressants, drugs that lower your immune system so it doesn't attack the new kidney as a foreign object. These aren't optional—they're life-long. Skipping even one dose can trigger rejection. Common ones include tacrolimus, mycophenolate, and prednisone. Each has side effects: weight gain, shaky hands, higher infection risk, or raised blood sugar. Your team will tweak doses over time, balancing protection against the transplant with minimizing harm to your body. You'll also need regular blood tests to check drug levels and kidney function. Missing appointments isn't just risky—it can cost you the transplant.
Rejection doesn't always mean pain or fever. Sometimes, it shows up as a tiny rise in creatinine levels during a routine blood test. That's why monitoring is non-negotiable. Signs like swelling, reduced urine output, fever, or tenderness near the transplant site need immediate attention. Most rejections happen in the first year, but they can show up years later. That’s why lifelong follow-up with your transplant center matters. And while the new kidney works, your old one? It stays in place unless it's causing infection or high blood pressure. You don't need to remove it.
Many people wonder if they can go back to dialysis if the transplant fails. Yes, you can. But it’s harder the second time around. Your body may have built up antibodies from the first transplant, making it tougher to find a matching donor later. That’s why protecting your new kidney is so critical. Avoid NSAIDs like ibuprofen, stay hydrated, don’t smoke, and get your flu shot every year. Your new kidney is a gift—but it needs you to show up every day.
What you'll find below are real, practical guides written for people living with a transplant or supporting someone who is. From managing side effects of anti-rejection drugs to understanding how infections can sneak up on you, these posts give you tools—not just theory. You’ll see how other patients handle medication schedules, what to do when lab results look off, and how to spot early warning signs before they become emergencies. This isn’t about hope. It’s about staying in control.
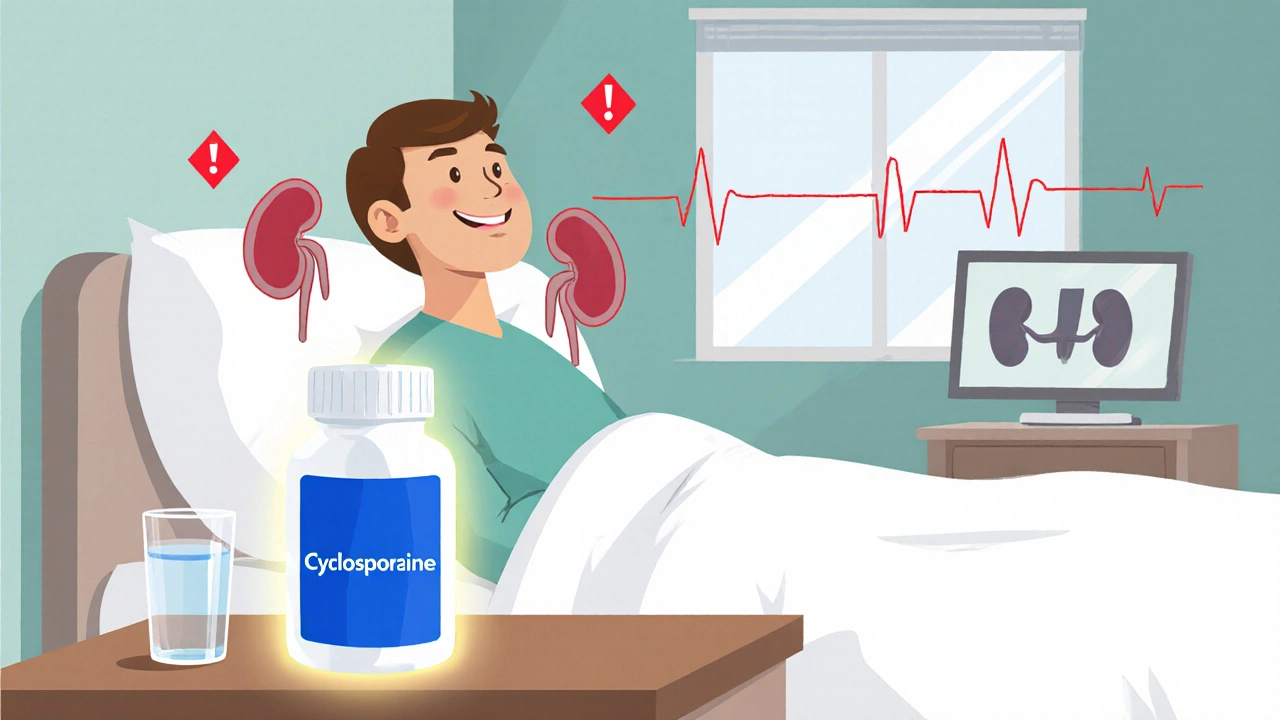
Cyclosporine Nephrotoxicity: How to Monitor Kidney Function & Drug Levels
- Laura Ledas
- Oct, 26 2025
Learn how to safely monitor cyclosporine levels and kidney function to avoid nephrotoxicity, with clear schedules, lab tips, and dose‑adjustment strategies.
Learn More