Disoproxil: What It Is and Why It Matters
When working with Disoproxil, a chemical moiety added to drugs to improve oral absorption and stability, you’re dealing with a key piece of modern pharmacy. Also called disoproxil fumarate, it turns poorly soluble compounds into forms the gut can pick up efficiently. In plain terms, Disoproxil acts like a carrier that helps the active ingredient slip through the intestinal wall, raising the amount that reaches the bloodstream.
How Disoproxil Connects to Antivirals and Prodrug Design
One of the most common pairings is Tenofovir, an antiretroviral nucleotide used to treat HIV and hepatitis B infections. By attaching Disoproxil to Tenofovir, manufacturers create Tenofovir disoproxil fumarate, a classic Prodrug, a chemically modified version of a drug designed to improve its pharmacokinetic profile. This prodrug strategy directly boosts Bioavailability, the proportion of a drug that enters circulation and can have an active effect. The semantic triple here is clear: Disoproxil enhances bioavailability, bioavailability improves therapeutic outcomes, and improved outcomes reduce dosing frequency. In practice, this means patients can take a single daily pill instead of multiple doses, simplifying adherence and cutting side‑effect risk.
Beyond Tenofovir, Disoproxil appears in other antiviral combos such as emtricitabine‑disoproxil and investigational hepatitis C agents. The chemistry behind the moiety involves an ester linkage that the body quickly cleaves, releasing the active drug once it’s absorbed. This rapid conversion is what makes the prodrug safe and effective: the ester itself is inert, and the released active compound reaches therapeutic levels faster than its raw form. Clinical guidelines therefore list Disoproxil‑based formulations as first‑line options for many viral infections because the enhanced absorption leads to steadier plasma concentrations and fewer resistance mutations.
Understanding how Disoproxil works also helps when evaluating drug interactions or switching therapies. Since the moiety relies on esterases in the gut and liver, drugs that inhibit these enzymes can slow the conversion process, potentially lowering efficacy. Conversely, substances that speed up metabolism might increase active drug levels and raise toxicity concerns. Knowing these relationships equips patients and clinicians to make informed choices about dosing, monitoring, and combination therapy. If you’re looking for practical advice, the articles below dive into related topics—alternative therapies for mental health, tapering guides for other medications, and safety tips for various drug classes. Together, they give a rounded view of how a single chemical trick like Disoproxil can shape treatment plans across many conditions.
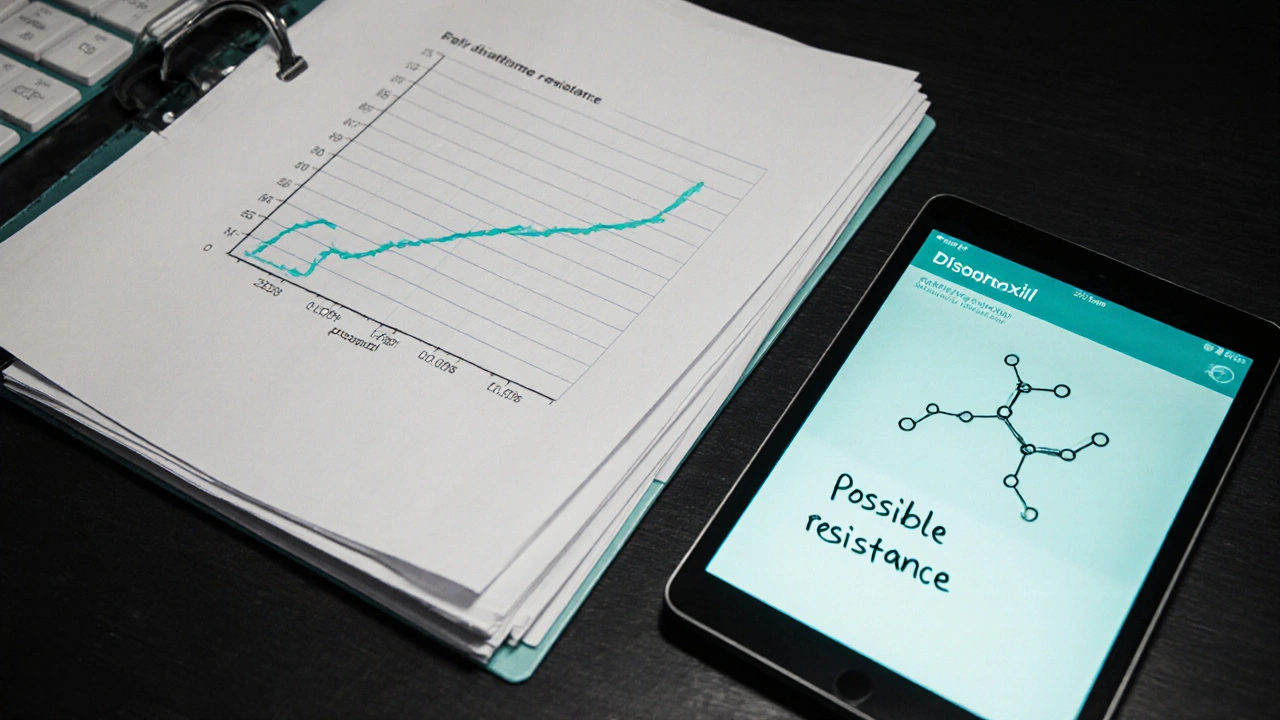
How to Manage Disoproxil Drug Resistance: Practical Strategies and Solutions
- Laura Ledas
- Oct, 6 2025
Learn how to detect, prevent, and treat Disoproxil drug resistance with clear strategies, monitoring tips, regimen switches, and a handy checklist.
Learn More