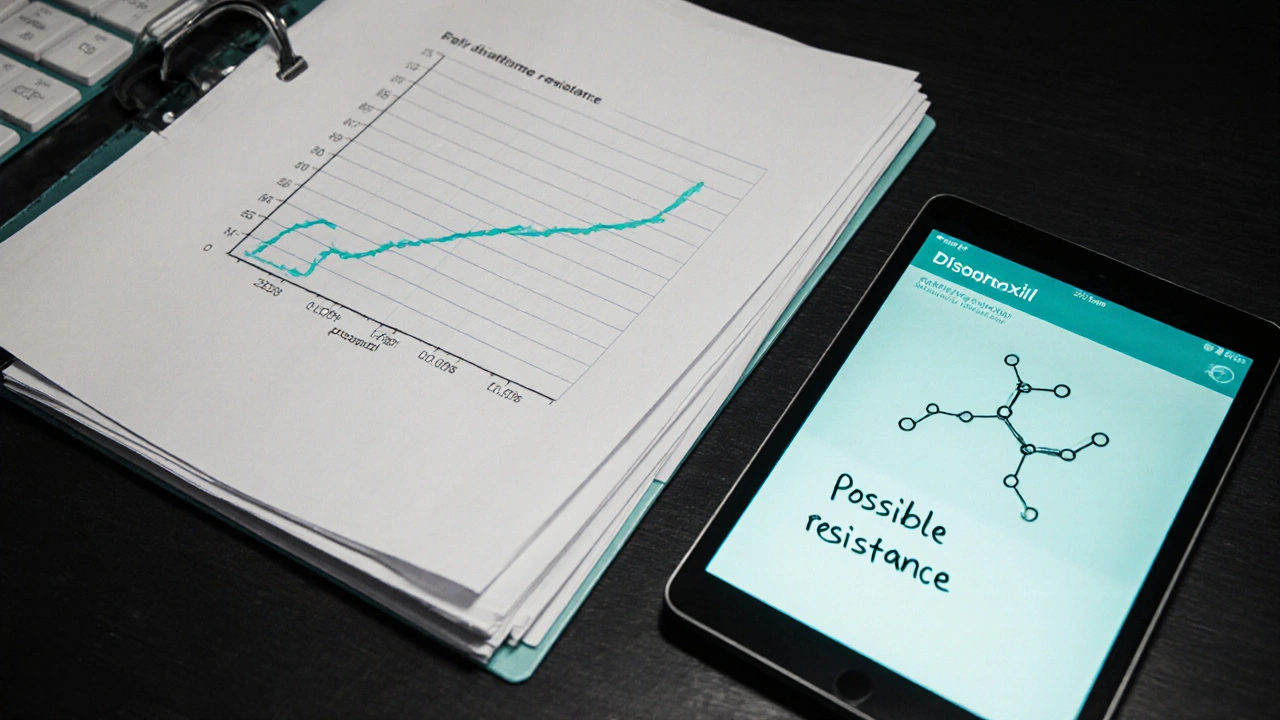
Disoproxil Resistance Calculator
Based on your selected resistance mutations, these treatment options remain effective:
Key Recommendations
- Optimize adherence to prevent further resistance
- Monitor renal function (eGFR) if continuing Disoproxil
- Consider switching to Tenofovir alafenamide (TAF) if K65R detected
- Add integrase strand transfer inhibitors (INSTIs) for high barrier to resistance
When a virus learns to sidestep a medication, patients can face treatment failure, higher viral loads, and faster disease progression. Disoproxil resistance isn’t just a lab‑side issue; it shows up in missed appointments, side‑effects, and confusing lab reports. This guide walks you through what drives resistance to Disoproxil, how to spot it early, and which moves clinicians and patients can make to stay ahead of the virus.
Key Takeaways
- Disoproxil (Tenofovir disoproxil fumarate) has a high genetic barrier but resistance can still emerge, especially with poor adherence.
- Routine viral load monitoring and genotypic resistance testing catch problems before they become clinical failures.
- Optimizing adherence, adjusting the background regimen, and considering newer prodrugs like Tenofovir alafenamide can restore viral suppression.
- Renal and bone health monitoring is essential when escalating or switching therapy.
- A simple checklist helps clinicians and patients act quickly when resistance is suspected.
Disoproxil is the pro‑drug form of tenofovir, marketed mainly as Tenofovir disoproxil fumarate (TDF). It works by mimicking natural nucleotides, getting incorporated into viral DNA and halting replication. Because it targets the reverse transcriptase enzyme, it’s a cornerstone of both HIV and chronic hepatitis B treatment.
Understanding Disoproxil Resistance
Resistance to Disoproxil usually stems from mutations in the viral reverse transcriptase gene. The most common HIV‑1 mutations are K65R, M184V/I, and thymidine analogue mutations (TAMs). While K65R reduces susceptibility to tenofovir, the presence of M184V can actually increase tenofovir’s effectiveness - a paradox that clinicians exploit when designing combination regimens.
In hepatitis B, resistance patterns differ; the rtA181V/T and rtN236T substitutions lessen tenofovir activity, but clinically significant resistance is rare compared with older nucleos(t)ide analogues.
When to Suspect Resistance
Early clues appear in routine labs:
- **Rising viral load** after at least three months of documented adherence (≥90%).
- **Persistently detectable viral load** (>200 copies/mL) on two consecutive tests spaced four weeks apart.
- **Clinical signs** such as unexplained CD4 decline in HIV or ALT elevation in hepatitis B.
When these signals surface, a genotypic resistance test should be ordered promptly. For HIV, the test reports specific mutations and their impact on each drug. For hepatitis B, sequencing of the polymerase region provides similar insight.

Optimizing Adherence - The First Line of Defense
Even the toughest drug can be outsmarted by missed doses. Strategies that consistently improve adherence include:
- **Fixed‑dose combinations** - pairing Disoproxil with emtricitabine (as in Truvada) reduces pill burden.
- **Mobile reminders** - SMS or app notifications synced with dosing times raise on‑time intake rates by up to 15%.
- **Medication lockers** - community pharmacies offering lockable, time‑release dispensers help patients who travel frequently.
- **Addressing side‑effects** - renal dysfunction or nausea often leads to self‑discontinuation; early lab checks and symptom management keep patients on track.
Adherence counseling should be documented at each visit, and any barriers (housing, mental health, substance use) must be tackled with referrals.
Adjusting the Regimen - What to Do When Resistance Is Confirmed
Once genotypic testing identifies resistance, clinicians have three main routes:
- Intensify the backbone. Adding a second NRTI with a different resistance profile (e.g., lamivudine when K65R is present) can restore full activity.
- Switch to a higher‑potency prodrug. Tenofovir alafenamide (TAF) delivers the same intracellular tenofovir diphosphate at lower plasma levels, reducing renal and bone toxicity while maintaining efficacy against K65R.
- Introduce a third‑class agent. Integrase strand transfer inhibitors (INSTIs) like dolutegravir have a high barrier to resistance and synergize well with tenofovir‑based backbones.
Choosing among these options depends on patient‑specific factors: existing comorbidities, renal function (eGFR), and prior exposure to other drug classes.
Renal and Bone Monitoring - Safety While You Fight Resistance
Disoproxil can affect kidneys and bone mineral density, especially at higher doses or in patients with pre‑existing conditions. Recommended monitoring schedule:
- Baseline serum creatinine and eGFR, then every 3months for the first year, followed by 6‑monthly checks.
- Baseline DEXA scan for patients over 50 or with osteoporosis risk; repeat every 2years if on long‑term therapy.
- Consider switching to TAF if eGFR falls below 60mL/min/1.73m² or if phosphorus loss becomes evident.

Comparison of Common Nucleos(t)ide Analogues
| Drug | Resistance Barrier | Renal Toxicity | Bone Impact | Typical Dose |
|---|---|---|---|---|
| Disoproxil (TDF) | High (but K65R reduces) | Moderate‑high | Moderate loss | 300mg daily |
| Tenofovir alafenamide (TAF) | High | Low | Low | 25mg daily |
| Lamivudine | Low (M184V) | Minimal | None | 150mg daily |
| Dolutegravir (INSTI) | Very high | Minimal | None | 50mg daily |
Practical Checklist for Managing Disoproxil Resistance
- 🔹 Verify ≥90% adherence over the past 3months.
- 🔹 Order a viral load test; if >200copies/mL on two occasions, proceed to genotypic testing.
- 🔹 Review renal function (eGFR) and bone density baseline.
- 🔹 If K65R detected, consider switching to TAF or adding an INSTI.
- 🔹 Counsel on side‑effect management; adjust dosing if nausea or GI upset persists.
- 🔹 Schedule follow‑up viral load in 4‑6weeks after any regimen change.
- 🔹 Document all decisions in the electronic health record with resistance rationale.
Next Steps & Troubleshooting
If viral suppression isn’t regained within 12weeks of a regimen switch, revisit the checklist:
- Re‑assess adherence - maybe a hidden barrier emerged after the switch.
- Repeat resistance testing - mixed‑virus populations can evolve under selective pressure.
- Check drug-drug interactions - certain antacids or calcium can lower Disoproxil absorption.
- Consider specialist referral - complex multi‑class resistance may need a resistance‑expert panel.
Frequently Asked Questions
Can I develop resistance to Disoproxil if I take it perfectly?
Even with perfect adherence, rare mutations like K65R can arise, especially after long‑term exposure. The risk stays low compared with older drugs, but clinicians still monitor viral load regularly.
Is Tenofovir alafenamide a safe alternative for patients with kidney disease?
TAF delivers the active metabolite inside cells, resulting in roughly 90% lower plasma tenofovir levels. For eGFR<60mL/min, switching to TAF is generally recommended, provided there are no contraindications.
How often should I get my viral load checked after a regimen change?
A repeat viral load is advised at 4‑6weeks post‑change, then again at 12weeks. If the result is <200copies/mL, continue routine 3‑monthly monitoring.
Do I need a bone density scan every year while on Disoproxil?
Annual DEXA isn’t required for most patients. Baseline testing, followed by a repeat every 2years-or sooner if risk factors (age>50, steroid use) appear-is the usual practice.
What should I do if my side‑effects prevent me from taking Disoproxil?
Report the symptoms immediately. Often, adjusting timing (taking with food), switching to TAF, or adding a brief renal‑protective supplement can alleviate issues without losing viral control.
10 Responses
Great rundown on the resistance pathways! 😊 Keeping adherence top of mind really does the heavy lifting when it comes to preventing K65R from taking hold. I’d also add that patients benefit from simple pill‑boxes and timed alarms to lock in the habit. Don’t forget to schedule renal labs every three months in the first year, especially if they’re on TDF. The checklist you posted makes it easy for clinicians to stay on track.
Monitoring eGFR regularly is a must when using Disoproxil.
The emphasis on early viral load spikes is spot on. Once you see two consecutive readings above 200 copies/mL, the genotypic test should be ordered without delay. I’ve seen patients who missed a single dose and still maintained suppression, but the real danger comes from chronic sub‑optimal adherence. Combining TDF with an INSTI like dolutegravir offers a high barrier and often rescues the regimen. Also, checking for drug‑drug interactions with antacids can save a lot of headaches later.
While the checklist is tidy, it glosses over the fact that many clinicians still cling to TDF despite its renal toxicity. Switching to TAF isn’t always the silver bullet; cost and insurance barriers can make it inaccessible for a large patient population. Moreover, the emphasis on adherence tools can feel patronizing to patients who already manage complex schedules. We need more pragmatic guidance on navigating these systemic hurdles.
Actually, the sentence “Switching to TAF isn’t always the silver bullet” should read “Switching to TAF isn’t always a silver bullet.” Also, “cost and insurance barriers can make it inaccessible” would be clearer as “cost and insurance barriers may render it inaccessible.” Precision matters when we’re discussing patient care.
Oh sure, just pop a cheap pill in the mailbox and the virus will magically disappear. It’s not like we need to think about resistance patterns or patient histories at all. Real world medicine rarely works that way, but hey, why not pretend?
You’re right that oversimplifying the issue is dangerous, but dismissing the whole guideline as “magic” ignores the solid data behind TAF and INSTI combinations. Patients need clear, evidence‑based steps, not just vague encouragement. If we want them to stick to therapy, we have to give them realistic options and address the barriers they actually face.
It’s disappointing how often clinicians treat resistance like an afterthought rather than a primary concern. The checklist is useful, but only if the provider actually reads it and applies it consistently. Too many providers assume good adherence without verifying it, leading to silent treatment failures. We need a cultural shift toward proactive resistance monitoring.
Managing Disoproxil resistance is a multifaceted challenge that extends far beyond simply swapping one drug for another. First, clinicians must recognize that adherence is the single most modifiable factor, and any intervention should begin with a thorough assessment of daily routines, socioeconomic pressures, and mental health status. Second, when resistance mutations like K65R or M184V are identified, the therapeutic strategy should be tailored to exploit the unique pharmacodynamics of each drug; for instance, the paradoxical increase in tenofovir efficacy in the presence of M184V can be leveraged by maintaining a robust backbone while adding a high‑barrier agent such as dolutegravir. Third, renal and bone health monitoring cannot be an afterthought; baseline eGFR and DEXA scans provide a reference point for detecting drug‑related toxicities early and making timely switches to lower‑toxicity alternatives like TAF. Fourth, the integration of electronic health record alerts for rising viral loads can prompt earlier genotypic testing, reducing the window in which resistant strains proliferate. Fifth, patient education should be an ongoing dialogue, employing visual aids and multilingual resources to ensure that individuals understand the significance of each lab result. Sixth, community pharmacy programs that dispense medication in pre‑filled, time‑release blister packs have demonstrated improved adherence in low‑resource settings. Seventh, drug‑drug interactions, especially with calcium or iron supplements, must be reviewed at each visit to prevent sub‑therapeutic absorption of Disoproxil. Eighth, when resistance persists despite optimal adherence and regimen adjustment, referral to a specialist resistance panel can uncover complex multi‑class resistance patterns that require novel combination strategies. Ninth, cost considerations are real; negotiating bulk purchasing agreements or patient assistance programs can make newer agents like TAF more accessible. Tenth, research continues to explore long‑acting injectable formulations that may eventually circumvent daily adherence challenges altogether. Eleventh, clinicians should document every decision point in the medical record, citing specific resistance mutations and the rationale for each drug change, which aids both continuity of care and medicolegal protection. Twelfth, interdisciplinary collaboration with pharmacists, social workers, and mental health professionals creates a safety net that catches adherence lapses before they translate into virologic failure. Thirteenth, regular audit of clinic outcomes related to resistance can highlight gaps in practice and drive quality improvement initiatives. Fourteenth, patient‑reported outcome measures can provide insight into tolerability issues that might otherwise go unrecognized. Finally, staying current with evolving guidelines and emerging data ensures that treatment plans remain evidence‑based and adaptable to the ever‑changing landscape of viral resistance.
Wow, that was an epic deep‑dive! 🚀💡 I love how you broke everything down into bite‑size steps and even tossed in some real‑world hacks. Definitely going to add the pharmacy blister pack tip to my notes – it’s a game‑changer. Your point about long‑acting injectables feels like the future we’ve been waiting for. Thanks for the marathon of wisdom! 🙌