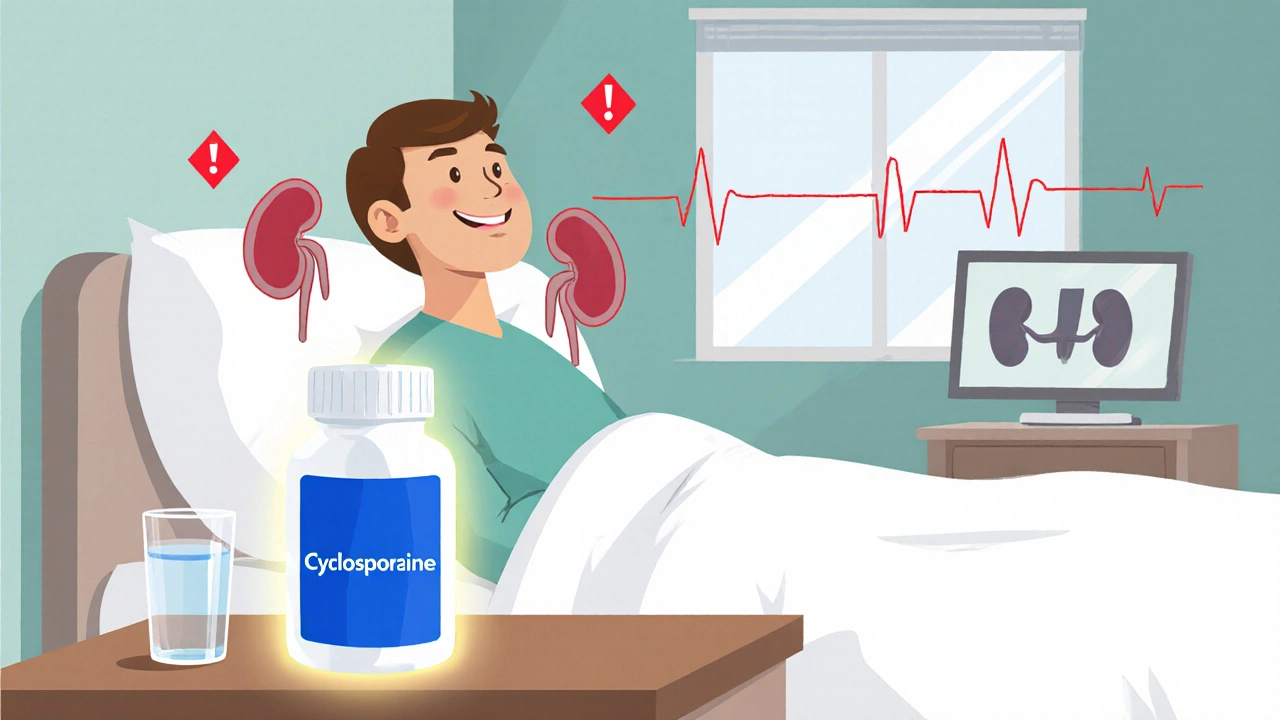
Cyclosporine Nephrotoxicity: Risks, Signs, and How to Protect Your Kidneys
When you take cyclosporine, an immunosuppressant used after organ transplants and for autoimmune conditions. Also known as CsA, it stops your immune system from attacking your new organ—but it doesn’t know when to stop hurting your kidneys. That’s where cyclosporine nephrotoxicity, kidney damage caused directly by cyclosporine comes in. It’s not rare. In fact, up to half of people on long-term cyclosporine show some sign of kidney stress. This isn’t just a lab number—it’s real, measurable harm that can lead to chronic kidney disease if unchecked.
This damage happens because cyclosporine narrows the tiny blood vessels inside your kidneys, reducing blood flow. Over time, that strain causes scarring and loss of filtering function. The risk goes up with higher doses, longer use, and if you already have high blood pressure, diabetes, or older age. It also gets worse if you’re taking other drugs that hurt the kidneys—like NSAIDs, certain antibiotics, or even some herbal supplements. Drug-induced kidney injury, a broad category that includes cyclosporine’s effects is often silent until it’s advanced. That’s why regular blood tests for creatinine and eGFR aren’t optional—they’re your early warning system.
You might not feel anything at first. No pain. No swelling. Just a slow drop in kidney function. But watch for subtle signs: swelling in your ankles, foamy urine, unusual fatigue, or high blood pressure that’s harder to control. These aren’t just side effects—they’re red flags. Your doctor should check your kidney levels every few weeks when you start cyclosporine, then at least every 3 months after that. Dose adjustments, switching to a different immunosuppressant like tacrolimus, or adding protective meds like calcium channel blockers can help. Lifestyle matters too: stay hydrated, avoid salt overload, and skip anything that stresses your kidneys.
What you’ll find below isn’t theory—it’s real guidance from people who’ve lived with this. You’ll see how others tracked their kidney numbers, what changes helped them avoid further damage, and how doctors adjusted treatment when things went sideways. Some switched meds. Others added supplements. A few learned to live with mild kidney changes without losing transplant function. These aren’t perfect stories—they’re practical ones. And they’re the kind of details you won’t find in a drug leaflet.
Cyclosporine Nephrotoxicity: How to Monitor Kidney Function & Drug Levels
- Laura Ledas
- Oct, 26 2025
Learn how to safely monitor cyclosporine levels and kidney function to avoid nephrotoxicity, with clear schedules, lab tips, and dose‑adjustment strategies.
Learn More