Glaucoma Medication Comparison Tool
Compare Your Glaucoma Treatment Options
Select medications to compare their key characteristics for glaucoma management.
Select two medications to view comparison
Key Takeaways
- Brimonidine tartrate is an alpha‑2 agonist that lowers intra‑ocular pressure (IOP) in glaucoma and ocular hypertension.
- It also helps with allergic conjunctivitis and offers neuroprotective effects.
- Typical dosing is one drop in each eye twice daily, but exact regimen depends on the condition.
- Common side effects are mild (dry eye, mild redness) while serious reactions are rare.
- When compared with beta‑blockers or prostaglandin analogues, brimonidine provides a different safety profile and can be combined with other drops.
When you hear the name brimonidine tartrate, think of a targeted eye‑drop solution that does more than just lower pressure. It’s a drug that balances efficacy, comfort, and a growing body of research on eye‑health protection.
What Is Brimonidine Tartrate?
Brimonidine tartrate is an alpha‑2 adrenergic agonist formulated as ophthalmic solution (eye drops) to reduce intra‑ocular pressure. First approved in the United States in 1996, it quickly became a cornerstone for managing open‑angle glaucoma and ocular hypertension. The molecule works by decreasing aqueous humor production and increasing uveoscleral outflow, which together lower the pressure inside the eye.
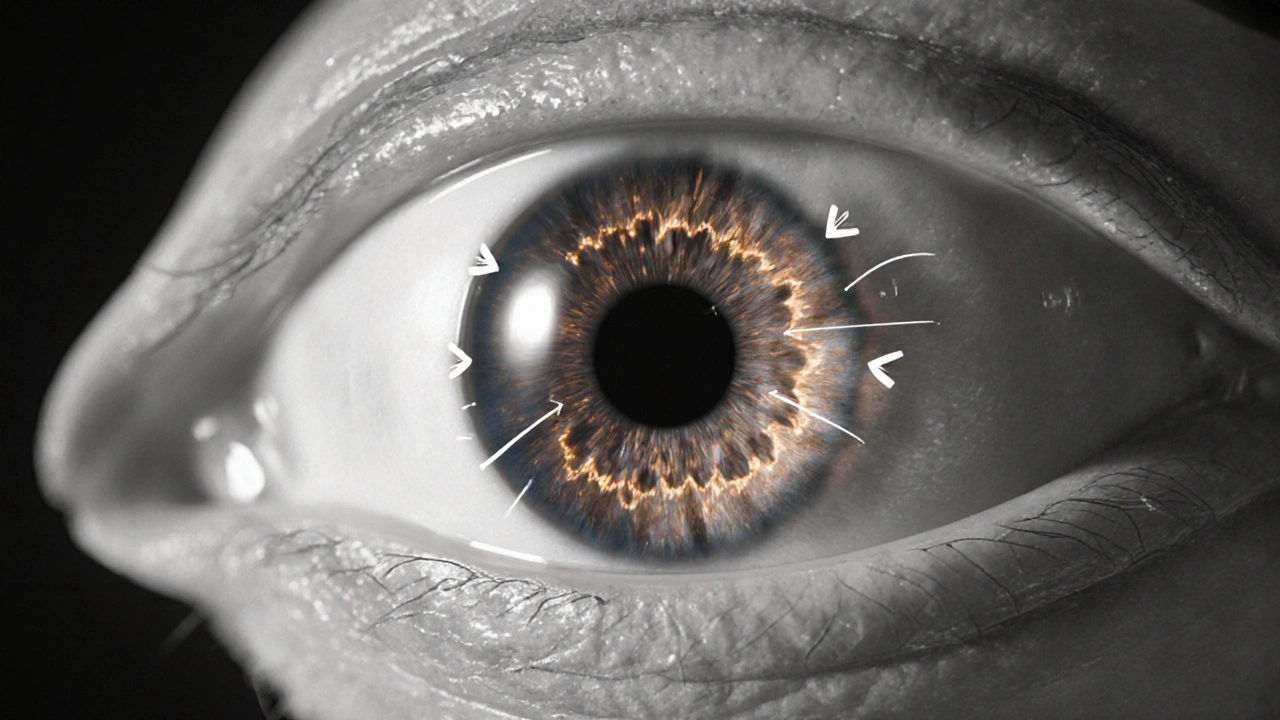
How It Works: The Alpha‑2 Mechanism
Alpha‑2 agonist is a class of drugs that stimulate alpha‑2 receptors in the ciliary body. When these receptors are activated, the eye reduces the amount of fluid (aqueous humor) that it creates. Less fluid means less pressure on the optic nerve, slowing the damage that leads to vision loss.
Primary Clinical Uses
- Glaucoma management: In primary open‑angle glaucoma, lowering IOP is the only proven way to prevent progressive vision loss. Brimonidine tartrate typically brings IOP down 20‑30% after the first week of treatment.
- Ocular hypertension: For patients with high eye pressure but no optic nerve damage yet, the drug helps keep pressure in a safe range.
- Allergic conjunctivitis: The formulation also contains an anti‑inflammatory effect that eases redness, itching, and tearing caused by allergens.
- Adjunct therapy: Because it works via a different pathway than beta‑blockers (e.g., timolol) or prostaglandin analogues (e.g., latanoprost), it can be combined for added pressure‑lowering power.
Benefits Over Other Eye‑Drop Options
When you compare brimonidine tartrate to other common ocular hypotensives, several advantages stand out:
- Neuroprotection refers to the drug’s ability to protect retinal ganglion cells from stress‑induced death. Laboratory studies suggest brimonidine may reduce cell loss independent of pressure reduction.
- It has a relatively short systemic absorption profile, so patients with asthma or certain heart conditions often tolerate it better than beta‑blockers.
- Preservative‑free formulations are now widely available, reducing the risk of ocular surface irritation for dry‑eye sufferers.
- Twice‑daily dosing fits easily into most daily routines, avoiding the nightly drop‑application challenge of some prostaglandin agents.
Dosage, Administration & Practical Tips
Correct technique maximizes benefit and minimizes waste. Follow these steps:
- Wash your hands thoroughly.
- Shake the bottle gently if the label says to do so.
- Tilt your head back slightly, pull down the lower eyelid to create a small pocket.
- Hold the bottle close to the eye (no more than 1‑2 cm) and press gently to release one drop.
- Close your eye lightly for about 30 seconds, pressing the inner corner (nasal canthus) to block tear drainage.
- Wait at least 5 minutes before applying any other eye medication.
Typical dosing is one drop in each affected eye twice daily (morning and early evening). Some clinicians start with once‑daily dosing for allergic conjunctivitis and step up if pressure control is insufficient.

Safety Profile & Common Side Effects
Most patients experience mild, transient symptoms. The most frequently reported effects include:
- Dryness or a gritty sensation
- Mild redness or conjunctival hyperemia
- Temporary blurred vision (usually clears within a few minutes)
Serious adverse events-such as severe allergic reactions, significant systemic hypotension, or worsening asthma-are rare but warrant immediate medical attention. Side effects are usually dose‑related and resolve when the medication is stopped or the dose is adjusted.
Comparison with Other Ocular Hypotensives
| Attribute | Brimonidine tartrate | Timolol (beta‑blocker) | Latanoprost (prostaglandin analogue) |
|---|---|---|---|
| Mechanism | Alpha‑2 agonist - reduces aqueous production & increases outflow | Beta‑blocker - reduces aqueous production | Prostaglandin analogue - increases uveoscleral outflow |
| Typical IOP reduction | 20‑30% | 20‑25% | 25‑30% |
| Dosing frequency | Twice daily | Twice daily | Once nightly |
| Systemic contraindications | Asthma, severe COPD (relatively safe) | Asthma, severe COPD, bradycardia | None significant; caution in pregnancy |
| Common ocular side effects | Dryness, mild redness | Blurred vision, sting | Eye darkening, eyelash growth |
| Neuroprotective evidence | Positive in animal & early human studies | Limited | Limited |
Frequently Asked Questions
Can I use brimonidine tartrate if I wear contact lenses?
Yes, but remove the lenses before instilling the drops, wait at least five minutes, then re‑insert. This prevents the medication from being trapped under the lens and reduces irritation.
How quickly does the pressure start to drop?
Most patients see an IOP reduction within 30‑60 minutes after the first dose, with a steady plateau after a week of consistent use.
Is it safe to use brimonidine with other glaucoma drops?
Because it works via a different receptor pathway, it is often combined with prostaglandin analogues or beta‑blockers for additive pressure control. Always follow your eye‑care professional’s schedule to avoid wash‑out.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and continue with your regular schedule-don’t double up.
Are there preservative‑free options?
Yes. Several manufacturers now offer preservative‑free brimonidine bottles or single‑use vials, which are ideal for patients with dry‑eye syndrome or sensitivity to benzalkonium chloride.
Understanding how brimonidine tartrate fits into an eye‑care regimen helps you or your loved one make informed choices. Whether you’re starting treatment for glaucoma, managing ocular hypertension, or looking for relief from allergic eye symptoms, the drug’s unique mechanism, safety profile, and emerging neuroprotective data make it a valuable option in modern ophthalmology.

9 Responses
Brimonidine’s dual action-cutting aqueous production while boosting outflow-makes it a solid choice when beta‑blockers are off‑limits. The twice‑daily schedule fits nicely into most morning and early evening routines, so adherence isn’t a huge hurdle. It’s also worth noting that the drug’s systemic absorption is minimal, which is why asthma patients often tolerate it better than timolol. For folks juggling multiple glaucoma meds, the non‑overlapping mechanism adds an extra pressure‑lowering punch without much added risk. Overall, it’s a versatile tool in the ophthalmic arsenal.
i luv the preservative‑free bottles they got now.
From a clinical perspective, brimonidine tartrate represents a noteworthy advancement in the management of open‑angle glaucoma and ocular hypertension. Its mechanism, centered on alpha‑2 adrenergic receptor stimulation, not only diminishes aqueous humor production but also enhances uveoscleral outflow, thereby delivering a comprehensive reduction in intra‑ocular pressure. Evidence from randomized controlled trials indicates a mean IOP decrement of approximately 20‑30 percent within the first week of therapy, a figure that is comparable to that achieved by traditional beta‑blockers and prostaglandin analogues. Moreover, brimonidine’s neuroprotective potential, demonstrated in both animal models and early human investigations, suggests an adjunctive benefit beyond mere pressure control, possibly preserving retinal ganglion cell integrity. The safety profile is generally favorable; systemic adverse events such as hypotension or bronchospasm are infrequent, owing to limited systemic absorption, which renders the drug particularly suitable for patients with respiratory comorbidities. Local ocular side effects are typically mild and transient, most commonly manifesting as dryness, a gritty sensation, or mild conjunctival hyperemia, all of which resolve spontaneously or with adjunctive lubricants. The twice‑daily dosing regimen, administered in the morning and early evening, aligns well with patient adherence patterns, especially when contrasted with the nightly application required for many prostaglandin agents. In addition, the availability of preservative‑free formulations mitigates the risk of ocular surface toxicity, a salient consideration for individuals with pre‑existing dry eye disease. When employed as part of a combination therapy strategy, brimonidine synergizes effectively with both beta‑blockers and prostaglandin analogues, offering additive pressure‑lowering effects without pharmacologic antagonism. It is therefore incumbent upon the prescribing clinician to evaluate the individual patient’s systemic health, ocular surface status, and dosing preferences when selecting brimonidine as part of a comprehensive glaucoma management plan. In summary, brimonidine tartrate provides a robust efficacy profile, a tolerable safety spectrum, and a unique neuroprotective attribute that collectively justify its inclusion among first‑line therapeutic options for glaucoma and ocular hypertension.
Wow, brimonidine actually helps with allergic conjunctivitis too! 😲 That’s a handy two‑for‑one. Plus, the double‑daily drops aren’t that big of a hassle compared to those nightly prostaglandins.
the drug works well but watch out for dry eyes. i had a bit of itch after a week, so i used artificial tears.
It is imperative to note that the term “twice daily” should be rendered as “twice‑daily” when used as a compound adjective preceding a noun, per the Chicago Manual of Style. Furthermore, the phrase “reduces aqueous humor production & increases outflow” would be more formally expressed as “reduces aqueous humor production and increases outflow.” Finally, citing peer‑reviewed literature rather than generic web links would substantiate the neuroprotective claims more robustly.
Considering the modest systemic absorption, brimonidine can be a prudent alternative for patients who cannot tolerate timolol due to respiratory concerns. The drug’s efficacy appears consistent across diverse demographics, suggesting a broad applicability.
The inclusion of preservative‑free formulations addresses a common source of ocular surface irritation, particularly for individuals with pre‑existing dry eye syndrome. By eliminating benzalkonium chloride, clinicians can reduce the incidence of conjunctival hyperemia and discomfort associated with chronic drop use. Moreover, the pharmacokinetic profile of brimonidine, characterized by a rapid onset of action within 30‑60 minutes, provides patients with prompt symptomatic relief, which is advantageous in acute pressure spikes. When combined with prostaglandin analogues, the additive effect on intra‑ocular pressure can achieve reductions exceeding 30 percent, thereby offering a more aggressive therapeutic strategy for advanced glaucoma cases. It is essential, however, to counsel patients on proper instillation technique, including nasolacrimal occlusion, to minimize systemic exposure and maximize ocular bioavailability. In practice, the drug’s safety profile, combined with its dual utility in glaucoma and allergic conjunctivitis, makes it a compelling component of a comprehensive eye‑care regimen.
From a therapeutic standpoint, brimonidine’s alpha‑2 agonist activity provides a distinct mechanistic pathway that complements existing beta‑blocker and prostaglandin treatments. This diversification is particularly valuable in multi‑modal regimens, where synergistic pressure reduction can be achieved without overlapping adverse effect profiles. Clinicians should remain vigilant for the occasional ocular surface dryness, which can be mitigated with adjunctive lubricants or preservative‑free preparations. The drug’s relative safety in patients with chronic obstructive pulmonary disease underscores its suitability for a broader patient population, especially when contraindications limit the use of timolol. Additionally, emerging data on neuroprotection, while still preliminary, suggest a potential role in preserving retinal ganglion cell function beyond intra‑ocular pressure management. As such, brimonidine may represent not only a pressure‑lowering agent but also a disease‑modifying therapy pending further investigation. Ultimately, individualized patient assessment, including systemic comorbidities, ocular surface health, and adherence considerations, will dictate the optimal placement of brimonidine within the glaucoma treatment algorithm.