Vitamin K Intake Calculator
Calculate Your Vitamin K Intake
Enter your daily portions of vitamin K-rich foods to track your intake consistency. Consistency is key for stable INR levels while on warfarin.
Important: Aim to keep your daily vitamin K intake within 20% of your usual amount. A sudden increase or decrease can cause dangerous INR fluctuations.
Your Vitamin K Intake
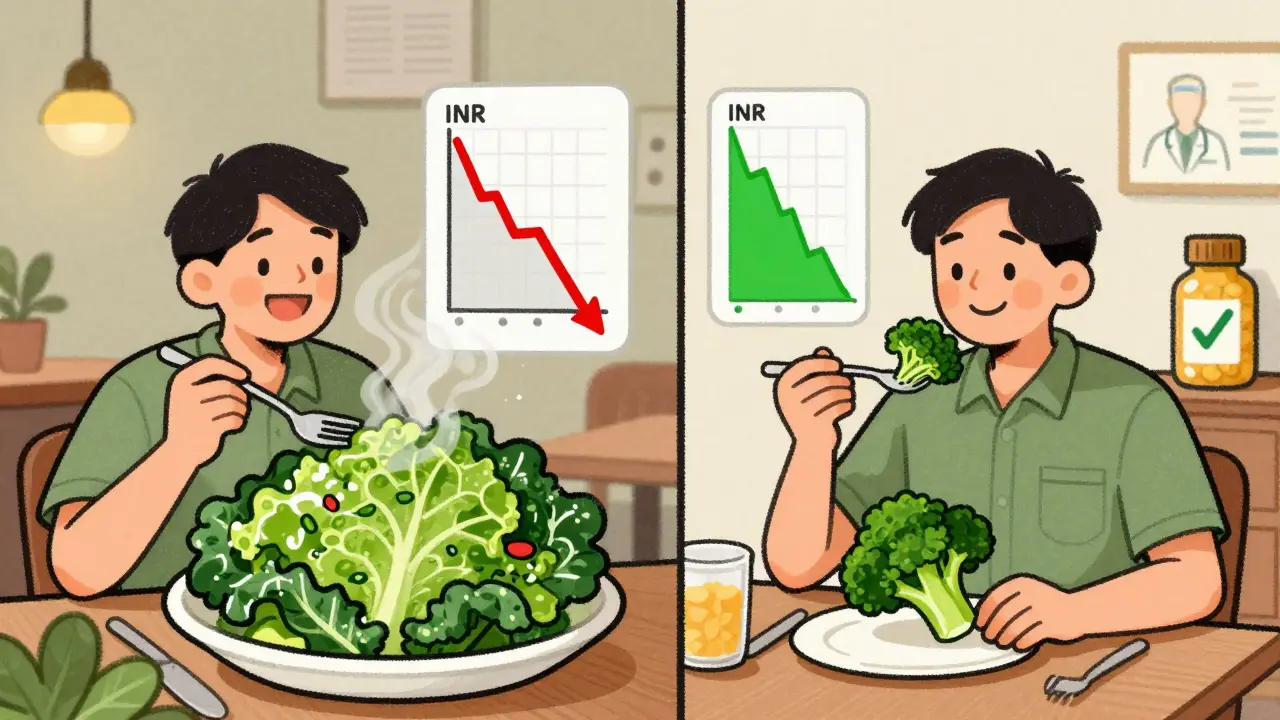
If you're taking warfarin, your diet isn't about cutting out healthy foods-it's about keeping things steady. One day you eat a big salad with kale and spinach; the next day you skip the greens entirely. That kind of swing can throw your blood clotting off balance, and it’s not just a small risk-it’s a real danger. You don’t need to avoid vitamin K-rich foods. You just need to eat about the same amount every day.
Why Vitamin K Matters When You're on Warfarin
Warfarin works by blocking vitamin K’s role in making clotting factors. Without enough active vitamin K, your blood takes longer to clot. That’s the whole point-it prevents dangerous clots from forming in your heart, legs, or lungs. But here’s the catch: if you suddenly eat a lot more vitamin K, your body gets more of what warfarin is trying to block. Your blood starts clotting faster again, and your INR drops. If your INR falls below 2.0, you’re at higher risk for stroke or pulmonary embolism.
On the flip side, if you eat way less vitamin K than usual-say, you go on a juice cleanse or cut out all vegetables-your blood thins too much. An INR above 3.0 increases your chance of bleeding, even from minor bumps or nosebleeds. Studies show that a change of just 100 micrograms of vitamin K in a single day can shift your INR by half a point or more. For someone with a target range of 2.0 to 3.0, that’s the difference between being protected and being at risk.
Which Foods Have the Most Vitamin K?
Vitamin K1, the kind you get from plants, is the main concern. It’s not in meat, dairy, or grains-it’s in leafy greens and some other vegetables. Here’s what’s packed with it:
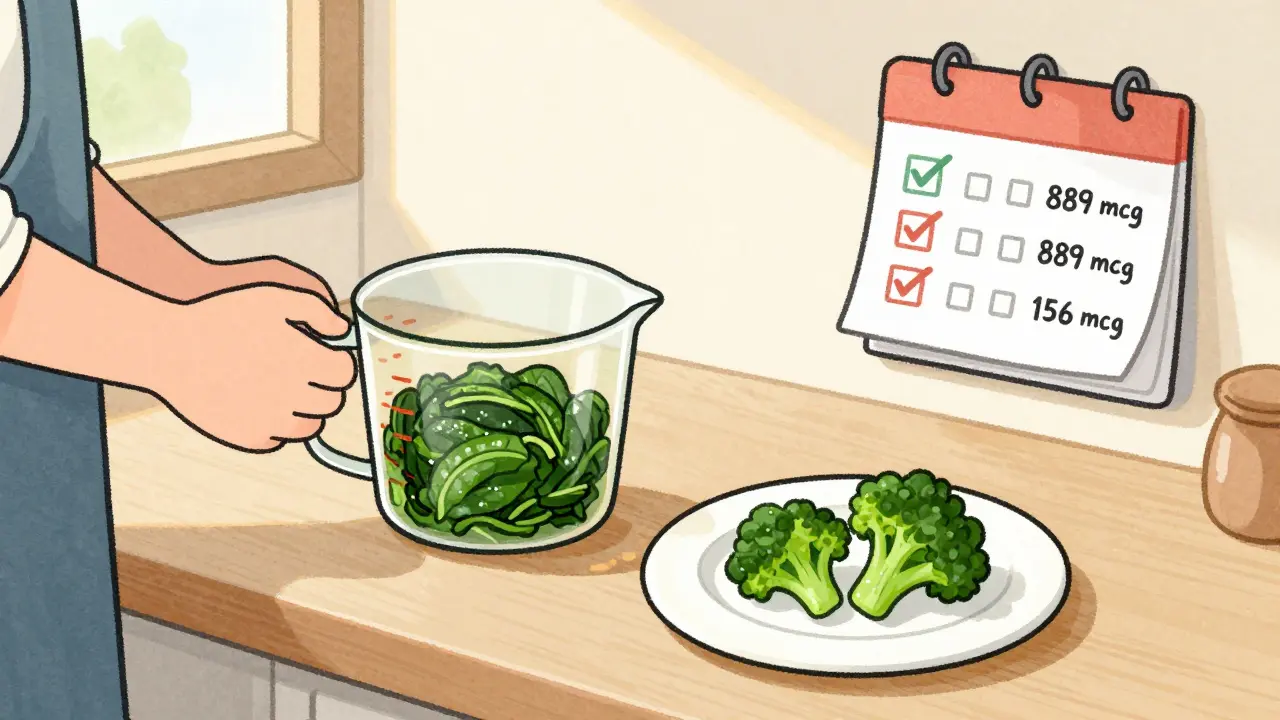
- Cooked kale: over 1,000 mcg per cup
- Cooked spinach: nearly 900 mcg per cup
- Raw Swiss chard: almost 300 mcg per cup
- Brussels sprouts: 156 mcg per cup
- Raw broccoli: 85 mcg per cup
- Asparagus: 70 mcg per cup
- Green tea: 41-88 mcg per serving
These aren’t obscure superfoods-they’re everyday vegetables. If you’ve ever eaten a green smoothie, a side of steamed broccoli, or a salad with kale, you’ve consumed a significant amount of vitamin K. The problem isn’t the food itself. It’s inconsistency. One week you’re eating two cups of spinach every day. The next week, you’re eating none. That’s what messes with your INR.
Consistency Over Restriction
Doctors used to tell people on warfarin to avoid greens altogether. That advice is outdated-and dangerous. Cutting out healthy foods leads to other problems: poor nutrition, constipation, and even higher blood pressure. The American Heart Association, the Anticoagulation Forum, and the Mayo Clinic all agree now: don’t avoid vitamin K. Keep it steady.
Think of it like this: your body needs a predictable amount of vitamin K to work with warfarin. If your intake stays within 20% of your normal daily amount, you’re far more likely to stay in the safe INR range. One study found that patients who kept their vitamin K intake consistent 80% of the time stayed in range 78% of the time. Those who swung wildly? Only 42% of their INRs were on target.
It’s not about eating less. It’s about eating the same. If you normally eat one cup of cooked spinach three times a week, keep doing that. Don’t double it on Monday because you’re feeling healthy. Don’t skip it for a week because you’re “taking a break.”
Real-Life Pitfalls and How to Avoid Them
People don’t realize how easy it is to mess this up. Here are common mistakes-and how to fix them:
- “I started eating healthier.” Many patients begin eating more salads, smoothies, or green juices after a diagnosis. Suddenly, their vitamin K intake triples. Result? INR drops. Solution: Talk to your doctor before changing your diet. If you want to eat more greens, increase them slowly and get your INR checked after two weeks.
- “I didn’t realize restaurant food had so much vitamin K.” A stir-fry with broccoli and bok choy, a side of steamed asparagus, or a spinach salad at a café can pack 200-500 mcg of vitamin K in one meal. If you usually eat low-vitamin K meals at home, this throws things off. Solution: Ask how dishes are prepared. Choose grilled chicken with rice instead of greens if you’re unsure.
- “I skipped my greens because I was traveling.” Seasonal changes, vacations, or busy weeks can lead to inconsistent eating. One patient’s INR spiked to 5.2 after a week of eating only bread and pasta on a road trip. Solution: Pack a small bag of frozen spinach or kale. You can microwave it in a hotel room. Or take a multivitamin with vitamin K every day, so your baseline stays even.
One woman in the Stop the Clot registry kept her INR stable for eight years by eating exactly two cups of cooked spinach every Tuesday and Thursday. No more, no less. She didn’t eat spinach on other days. That’s consistency. That’s control.
What You Can Do to Stay on Track
Here’s a simple plan to keep your vitamin K intake steady:
- Track your intake. Use a food diary or a free app like MyFitnessPal. Write down the leafy greens and vegetables you eat each day. Don’t guess-measure with a cup.
- Choose one or two consistent sources. Pick one or two vitamin K-rich foods you like and stick to them. If you like broccoli, have half a cup every day. If you prefer kale, have one cup twice a week. Don’t switch between five different greens.
- Use measuring cups. A handful of spinach isn’t the same as a cup. A cup of raw spinach has about 145 mcg. A cup of cooked spinach has 889 mcg. That’s a six-fold difference. Always measure.
- Take your multivitamin daily. If you take one, make sure it has vitamin K and take it at the same time every day. Skipping it or switching brands can cause fluctuations.
- See a dietitian. If you’re struggling, ask your doctor for a referral to a registered dietitian who specializes in anticoagulation. Patients who get this help stay in range 85% of the time-much better than standard care.
What If You Eat Too Much Vitamin K?
Accidents happen. Maybe you ate a giant kale salad at a friend’s house. Or you had a green smoothie for breakfast and didn’t realize how much vitamin K was in it. What now?
If you eat more than double your usual amount, don’t panic. But do call your clinic. Your provider might suggest a small increase in your warfarin dose the next day-usually 10-20% higher-based on your INR history. Never adjust your dose on your own.
If your INR goes too high (above 10) and you’re not bleeding, your doctor might give you 1-2.5 mg of oral vitamin K to bring it down quickly. This isn’t a cure-it’s a safety net. The goal is to prevent the situation in the first place.
What About Vitamin K2?
Vitamin K2, found in fermented foods like natto, cheese, and egg yolks, is less of a concern. It makes up only about 10% of dietary vitamin K in Western diets. While it plays a role in bone and heart health, it doesn’t interfere with warfarin as much as K1. You don’t need to avoid cheese or eggs. Just keep your intake consistent, like you do with greens.
When to Get Your INR Checked
Once you’re stable, you’ll usually get your INR tested every 2-4 weeks. But if you’ve made any change to your diet-added a new vegetable, started a new supplement, or skipped your usual greens for more than two days-get tested sooner. Don’t wait for your next scheduled test.
Also, if you get sick, start a new medication, or change your alcohol intake, your INR can shift. Warfarin interacts with many antibiotics, painkillers, and even herbal supplements like garlic or ginseng. Always tell your doctor what you’re taking.
It’s Not Perfect-But It’s Manageable
Living on warfarin isn’t easy. It requires attention. But it’s not impossible. Thousands of people do it every day. You don’t need to eat bland food. You don’t need to give up your favorite meals. You just need to be aware of what’s in your food-and keep it steady.
Think of it like managing your blood pressure or diabetes. It’s not about perfection. It’s about routine. Eat your spinach the same way, the same amount, most days. Your body will thank you. Your INR will stay in range. And you’ll reduce your risk of both clots and bleeding.
Can I eat spinach if I’m on warfarin?
Yes, you can eat spinach-but keep the amount consistent. One cup of cooked spinach has nearly 900 mcg of vitamin K. If you normally eat one cup three times a week, keep doing that. Don’t suddenly eat three cups one day and none the next. Consistency matters more than avoiding it.
Should I avoid all green vegetables on warfarin?
No. Avoiding greens can lead to poor nutrition and doesn’t improve INR control. The goal is to eat about the same amount of vitamin K every day, not to eliminate it. Leafy greens are healthy. Just be consistent with how much you eat.
What happens if I eat too much vitamin K?
Eating a lot of vitamin K can lower your INR, making your blood clot faster. This increases your risk of stroke or clotting in your legs or lungs. If you eat a huge amount-like a big kale salad-you should contact your doctor. They may adjust your warfarin dose slightly, but never change it yourself.
Does vitamin K from supplements affect warfarin?
Yes. If you take a multivitamin or vitamin K supplement, it can affect your INR. If you take one, make sure it’s the same brand and dose every day. Skipping it or switching brands can cause your INR to swing. Talk to your doctor before starting any new supplement.
How often should I get my INR checked?
When stable, every 2-4 weeks. But if you change your diet, start a new medication, get sick, or miss your usual vitamin K foods, get tested sooner. Don’t wait for your next scheduled test.
Can I drink alcohol while on warfarin?
Moderate alcohol is usually fine-one drink a day. But heavy or binge drinking can increase your INR and raise bleeding risk. Also, alcohol can interfere with how your liver processes warfarin. Keep your intake consistent. Don’t drink heavily one week and not at all the next.
Do I need to see a dietitian?
Not everyone does, but it helps. Patients who work with a dietitian who understands anticoagulation stay in their target INR range 85% of the time-compared to 65% with standard care. If you’re struggling to keep your diet steady, ask your doctor for a referral.
Next Steps: Start Small, Stay Consistent
Don’t try to overhaul your diet overnight. Pick one thing: maybe it’s measuring your spinach, or taking your multivitamin every day at breakfast. Track it for a week. Then add another habit. Slowly, it becomes routine.
Warfarin isn’t a life sentence to restriction. It’s a reminder to pay attention-to your food, your body, and your health. With consistency, you can eat well, stay safe, and live fully.
9 Responses
Stop the nonsense. You don't need a PhD to eat the same amount of spinach every week. Just do it.
It is imperative to underscore that the prevailing clinical consensus, as articulated by the American Heart Association and corroborated by the Anticoagulation Forum, unequivocally rejects the antiquated notion of vitamin K restriction. Rather, the cornerstone of safe anticoagulation therapy lies in the meticulous maintenance of dietary vitamin K intake within a narrow, predictable range-ideally fluctuating no more than 20% from baseline. Deviations exceeding this threshold precipitate clinically significant INR instability, thereby elevating the risk of both thromboembolic and hemorrhagic events. The data are unequivocal: patients who adhere to consistent intake patterns exhibit INR stability in 78% of measurements, whereas those who oscillate between extremes achieve target ranges in a mere 42%. This is not a matter of dietary preference; it is a matter of pharmacokinetic precision.
...and yet... no one mentions that vitamin K1 is structurally distinct from K2... and that K2, while less potent, is bioavailable in fermented foods... and that some studies suggest K2 may actually improve vascular calcification... but no... we're all just supposed to eat spinach like robots... while ignoring the fact that your liver stores vitamin K for weeks... so maybe... just maybe... consistency isn't as critical as we've been told?... Or is it?... I don't know anymore...
my friend got her inr to 8.2 after eating a kale smoothie and they said it was her fault... but then she found out her doctor had switched her meds without telling her... and now she's scared to eat anything green... like... what even is real anymore? also i think the fda is hiding something about vitamin k... why do you think they don't label it on menus?... just saying...
It's funny how we treat warfarin like it's some mystical potion that only works if you eat the exact same amount of spinach every Tuesday... like your body's a thermostat and vitamin K is the dial... but here's the thing: you're not a machine... you're a human... with moods... with travel... with grief... with birthdays... and if you miss your spinach one week because you were burying your mom... should you die because you didn't measure it in cups?... maybe the real problem isn't your diet... it's that we've turned survival into a spreadsheet...
I take warfarin and eat curry with spinach every day. Same amount. No problems. Simple. No need to overthink.
so you're telling me i can't just eat a salad once a week like a normal person? and i have to measure it? like with a cup? what is this, prison? also i think the whole thing is a scam to sell apps and dietitians.
You got this. Start with one thing-maybe just measuring your spinach for a week. You don't have to be perfect. Just show up. Your body will thank you.
I'm from India, and we eat a lot of spinach in curries-every single day, same portion. Never had an issue. The key is routine, not fear. Keep it simple, keep it steady. That's all.