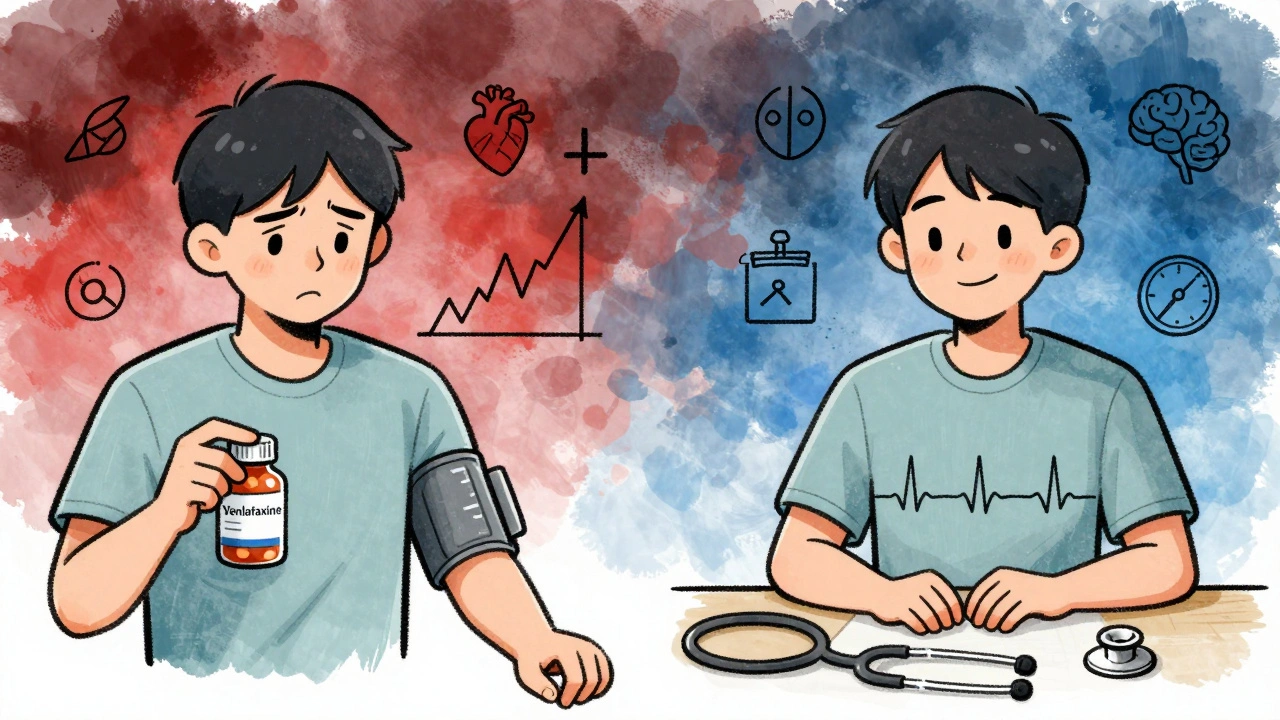
When you start taking venlafaxine for depression or anxiety, your doctor focuses on your mood. But there’s another number you need to watch - your blood pressure. Unlike many other antidepressants, venlafaxine doesn’t just affect your brain chemistry. It can raise your blood pressure, sometimes significantly. This isn’t rare. It’s well-documented. And if you ignore it, it can turn dangerous.
Why Venlafaxine Raises Blood Pressure
Venlafaxine, sold under brands like Effexor and Effexor XR, is an SNRI - a serotonin-norepinephrine reuptake inhibitor. That means it boosts two brain chemicals: serotonin and norepinephrine. Serotonin helps with mood. Norepinephrine? It’s your body’s natural stress hormone. It tightens blood vessels, speeds up your heart, and pushes blood pressure higher.
The more venlafaxine you take, the more norepinephrine builds up. Below 150 mg per day, the effect is mild. But once you hit 150 mg or more, the norepinephrine boost kicks in hard. Studies show that at doses above 300 mg/day, over 13% of people develop clinically high blood pressure - compared to just 5% on placebo. That’s not a small risk. That’s a real medical concern.
It’s not just about the dose, though. Some people - even young, healthy ones - develop sharp spikes in blood pressure at low doses. One case report described a 23-year-old man whose blood pressure shot to 210/170 mmHg after just 10 months on 150 mg. That’s a hypertensive crisis. He had no history of high blood pressure before starting venlafaxine. This isn’t theoretical. It’s happened.
How High Is Too High?
Most people on venlafaxine see a slow, steady rise - maybe 1 to 3 mmHg in diastolic pressure. That’s not alarming. But for some, it’s more. The average increase can reach up to 15 mmHg over time. That’s enough to push someone from normal (120/80) into the hypertensive range (140/90 or higher).
Here’s what the numbers mean:
- Normal: Below 120/80 mmHg
- Elevated: 120-129/<80 mmHg
- Stage 1 Hypertension: 130-139/80-89 mmHg
- Stage 2 Hypertension: 140+/90+ mmHg
- Hypertensive Crisis: 180+/110+ mmHg - seek emergency care immediately
Patients on venlafaxine have reported readings like 152/98 after just three weeks on 75 mg. That’s not an outlier. It’s a pattern. And it doesn’t always go away on its own.
How It Compares to Other Antidepressants
Not all antidepressants affect blood pressure the same way. SSRIs like sertraline or fluoxetine rarely cause any change. In fact, they’re often preferred for people with heart conditions because they’re safer.
Venlafaxine is different. It’s stronger than SSRIs for treatment-resistant depression - which is why doctors still prescribe it. But that strength comes with a trade-off. Compared to tricyclic antidepressants (TCAs), venlafaxine doesn’t cause dizziness from low blood pressure. Instead, it pushes pressure up. And unlike duloxetine - another SNRI - venlafaxine has a clearer, more consistent link to hypertension.
Even its metabolite, desvenlafaxine, raises blood pressure. Studies show a 0.66 to 3.41 mmHg rise in diastolic pressure at low doses. So if you switch from venlafaxine to desvenlafaxine thinking you’re avoiding the risk, you’re not.
Who’s at Risk?
Anyone taking venlafaxine could develop higher blood pressure. But some people are more vulnerable:
- Those already diagnosed with hypertension
- People over 65
- Those with kidney disease or diabetes
- Anyone taking other medications that raise blood pressure (like decongestants or stimulants)
- People on doses above 150 mg/day
Here’s something surprising: venlafaxine doesn’t make preexisting hypertension worse in most cases. In fact, some patients with unstable blood pressure report it actually becomes more stable on venlafaxine. But that’s not the norm. For most, the risk is a new rise - not a worsening of an old problem.

What Your Doctor Should Do
Guidelines are clear. Blood pressure monitoring isn’t optional - it’s required.
The American Psychiatric Association recommends:
- Baseline blood pressure check before starting venlafaxine
- Follow-up at 2 weeks and 4 weeks after starting
- Monthly checks for the first 3 months if you’re on more than 150 mg/day
- Quarterly checks after that
The Mayo Clinic adds: if your blood pressure rises above 140/90, your doctor should consider lowering your dose or switching meds. Don’t wait for symptoms. Don’t assume it’s just stress. Get it checked.
And if your BP hits 180/110 or higher? Go to the ER. That’s not a doctor’s appointment. That’s an emergency. High blood pressure from venlafaxine can lead to stroke, heart attack, or posterior reversible encephalopathy syndrome (PRES) - a rare but serious brain condition caused by sudden pressure spikes.
What You Should Watch For
You don’t always feel high blood pressure. That’s why it’s called the silent killer. But some signs can’t be ignored:
- Severe headache, especially at the back of your head
- Nosebleeds you can’t stop
- Blurred vision or seeing spots
- Chest pain or shortness of breath
- Dizziness or confusion
One patient described a nosebleed that wouldn’t stop after starting venlafaxine. That was her first clue. Another felt like her heart was pounding even when sitting still. These aren’t normal side effects. They’re warning signs.
What Happens If You Stop?
Good news: if venlafaxine is the cause, your blood pressure usually drops back to normal. Most people see improvement within 1 to 4 weeks after stopping. One Reddit user reported his BP went from 155/102 back to 120/80 after discontinuing the drug. No medication needed.
But don’t quit cold turkey. Withdrawal can cause dizziness, nausea, and brain zaps. Work with your doctor to taper slowly. If your BP stays high after stopping, there’s another issue - and you need to find it.
Real Stories, Real Risks
On patient forums, stories pour in:
- “I started 75 mg for anxiety. Three weeks later, my BP was 152/98. My doctor said it was the drug. I stopped. Two weeks later, I was back to normal.”
- “I’ve had high BP for years. My psychiatrist said venlafaxine would be fine. It wasn’t. My numbers kept climbing until I switched to sertraline.”
- “I was on 300 mg. My BP was 160/100. I didn’t feel different. My doctor didn’t check it until my annual physical. That’s when we found out.”
These aren’t rare. In one online forum with 147 responses, 68% of users reported higher blood pressure. Twelve percent had readings above 140/90. That’s nearly 1 in 8 people.
On Drugs.com, 28% of negative reviews mention blood pressure. That’s the third most common complaint after weight gain and sexual side effects.
Is It Still Worth Taking?
Yes - if you’re monitored.
Venlafaxine works where other antidepressants fail. For treatment-resistant depression, it’s one of the most effective options. The American Heart Association calls it a “reasonable alternative” when SSRIs don’t work. But they also say: mandatory monitoring is non-negotiable.
If you’re young, healthy, and have no history of heart issues, the risk is low - but not zero. If you’re over 50, have high cholesterol, or smoke? The risk is higher. Talk to your doctor about alternatives. Maybe sertraline, escitalopram, or even therapy combined with a different medication.
Don’t let fear stop you from getting help. But don’t let silence let it kill you.
What to Do Next
Here’s your action plan:
- If you’re starting venlafaxine: Ask for a baseline BP reading before your first dose.
- Buy a home blood pressure monitor. Check it weekly for the first month. Write down the numbers.
- Set calendar reminders for your follow-up appointments. Don’t wait for your doctor to ask.
- Know your numbers. If your systolic is over 140 or diastolic over 90, call your doctor - don’t wait.
- If you’re already on venlafaxine and haven’t had your BP checked in 6 months? Schedule an appointment today.
Venlafaxine saved lives. But it can also end them - if no one’s watching the numbers.
Can venlafaxine cause high blood pressure even at low doses?
Yes. While higher doses (above 150 mg/day) are more likely to raise blood pressure, cases have been documented where patients developed severe hypertension - including readings over 200/120 - at doses as low as 75 mg or 150 mg. This is rare but serious. It’s not just about the dose - some people are more sensitive to the norepinephrine effects. That’s why baseline and regular monitoring are essential, no matter the dose.
How long does it take for blood pressure to rise after starting venlafaxine?
Blood pressure can rise within the first 2 to 4 weeks of starting venlafaxine. Some patients report spikes as early as 10 days after beginning treatment. The increase is often gradual, but in rare cases, it happens suddenly. That’s why doctors recommend checking blood pressure at 2 weeks and again at 4 weeks after starting - even if you feel fine.
Does venlafaxine affect everyone the same way?
No. Genetics, age, existing health conditions, and even how your body metabolizes the drug play a role. Some people see no change in blood pressure. Others see a small rise. A small percentage develop dangerous spikes. There’s no way to predict who will be affected - which is why everyone on venlafaxine needs monitoring. It’s not about risk level; it’s about safety.
Can I switch to another antidepressant if my blood pressure rises?
Yes. If your blood pressure rises significantly and stays high after dose adjustments, switching to an SSRI like sertraline or escitalopram is often the next step. These drugs rarely affect blood pressure and are just as effective for many people. Never stop venlafaxine abruptly - work with your doctor to taper safely while starting the new medication.
Is it safe to take venlafaxine if I already have high blood pressure?
It can be - but only if your blood pressure is well-controlled and you’re under close monitoring. Studies show venlafaxine doesn’t worsen hypertension in patients whose blood pressure is already managed with medication. But if your BP is uncontrolled (above 140/90), most doctors will avoid venlafaxine and choose an SSRI instead. Always tell your prescriber your full medical history - including any heart conditions or medications you’re taking.

8 Responses
omg i started venlafaxine last month and my bp spiked to 145/92 at my checkup i thought it was just stress but now i get it
i was skeptical at first but after my doc told me to monitor my bp daily i realized how real this is
my numbers went from 118/76 to 138/88 in 6 weeks
we lowered my dose and boom-back to normal
seriously, dont ignore this
the mechanism is clear-norepinephrine’s vasoconstrictive effect is dose-dependent and well-documented in the FDA labeling and clinical trials
patients on >150 mg/day need monthly bp checks, especially if they have any cardiovascular risk factors
this isn’t speculation, it’s pharmacology
so you’re telling me my 23-year-old cousin’s hypertensive crisis was because he took antidepressants and not because he drinks 5 energy drinks a day?
bro the SNRI class has a noradrenergic effect, period
venla = norepi booster, ssris = serotonin only
if you’re on 225+ mg and your bp’s creeping up, it’s not coincidence, it’s chemistry
also, if you’re not checking it at home, you’re flying blind
Monitoring blood pressure is essential when initiating venlafaxine therapy
Physicians must educate patients on potential hypertensive effects
Regular assessment prevents adverse outcomes
why are we letting big pharma push this crap on people
my uncle died from a stroke on this stuff
usa needs to ban this and go back to therapy
okay but have you heard about the woman in Ohio who went from 110/70 to 220/140 on 75 mg?
she was fine until day 17
her cardiologist said it looked like a horror movie
she’s now on bupropion and her bp is perfect
but she cried for three weeks because she thought she was losing her mind
and no one told her this could happen
so if you’re reading this and you’re on venlafaxine
go buy a home monitor today
your future self will thank you