Triple-negative breast cancer (TNBC) doesn’t respond to hormone therapy or HER2-targeted drugs. That leaves chemotherapy as the main tool - but even that isn’t enough for many patients. About 1 in 7 breast cancers is triple-negative, and it’s more likely to come back within the first few years after treatment. The good news? The landscape is changing fast. New treatments, smarter combinations, and personalized approaches are giving patients better odds than ever before.
What Makes Triple-Negative Breast Cancer Different?
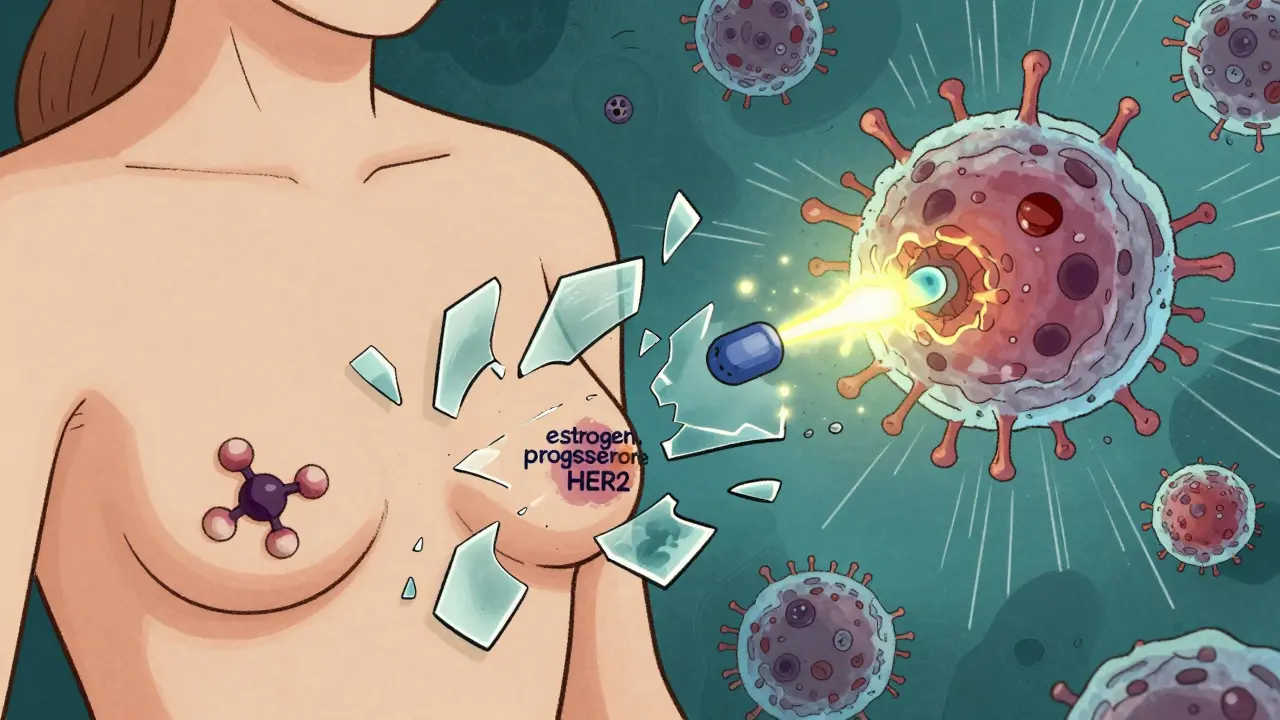
TNBC is defined by what it doesn’t have: no estrogen receptors, no progesterone receptors, and no excess HER2 protein. That means the drugs that work for other types of breast cancer - like tamoxifen or trastuzumab - just don’t work here. It’s not a single disease, but a group of aggressive tumors with different biology. That’s why some patients respond well to chemo while others don’t.
Because it grows quickly and spreads early, TNBC is often diagnosed at a later stage. About 15-20% of TNBC patients carry a germline BRCA1 or BRCA2 mutation, which affects how the cells repair DNA damage. That’s a key clue for treatment. Another 40% have PD-L1 expression on immune cells, which opens the door to immunotherapy. The rest? They’re still waiting for targeted options.
Standard Treatment: Chemo Still Leads, But It’s Evolving
For early-stage TNBC, the standard starts with neoadjuvant chemotherapy - meaning chemo before surgery. The goal isn’t just to shrink the tumor; it’s to get a pathologic complete response (pCR), which means no live cancer cells are found in the breast or lymph nodes after treatment. Patients who reach pCR have much better long-term survival.
Common regimens include anthracyclines like doxorubicin and taxanes like paclitaxel. But platinum drugs - cisplatin or carboplatin - are now routinely added, especially for those with BRCA mutations. In the GeparNuevo trial, adding the immunotherapy drug durvalumab to chemo raised the 3-year survival rate to 92.5%, compared to 83.5% with chemo alone.
After surgery, some patients get more chemo (adjuvant therapy), especially if they didn’t achieve pCR. But here’s the shift: we’re starting to ask, Can we do less? A 2025 study from UT Southwestern Medical Center showed that giving radiation at the very start of treatment, followed by just two doses of pembrolizumab and then chemo, achieved the same pCR rate (59%) as the standard KEYNOTE-522 protocol - but with only 41% serious side effects, compared to 82%.
Immunotherapy: Turning the Body’s Defenses Against Cancer
Immunotherapy works best when the tumor has signs of immune activity - like PD-L1 expression. For metastatic TNBC with PD-L1 CPS ≥10, pembrolizumab (Keytruda) combined with chemo became the first-line standard after the KEYNOTE-522 trial showed a 64.8% pCR rate in PD-L1-positive patients versus 44.1% in those without PD-L1.
Another option is atezolizumab (Tecentriq) with nab-paclitaxel, approved after the IMpassion130 trial showed a median progression-free survival of 7.2 months versus 5.5 months with chemo alone. These aren’t cures, but they give patients more time - and better quality of life - than chemo alone.
What’s new? Timing matters. The UT Southwestern approach shows that giving immunotherapy early and sparingly - just two doses - can be just as effective as months of treatment. This cuts down on fatigue, rashes, and immune-related side effects that can last for months.
Targeted Therapies: BRCA Mutations and PARP Inhibitors
If you have a BRCA1 or BRCA2 mutation - which is common in TNBC - PARP inhibitors like olaparib (Lynparza) and talazoparib (Talzenna) are game-changers. These drugs block a backup DNA repair system cancer cells rely on when BRCA is broken. In the OlympiAD trial, olaparib improved progression-free survival by 7.8 months compared to standard chemo.
It’s not just BRCA. Tests for homologous recombination deficiency (HRD) are now being used to find more patients who might benefit from PARP inhibitors, even without a clear BRCA mutation. That’s expanding the pool of people who can use these drugs.
Antibody-Drug Conjugates: Precision Bombs for Cancer Cells
Sacituzumab govitecan (Trodelvy) is an antibody-drug conjugate (ADC) that delivers a powerful chemo drug directly to cancer cells. It targets TROP-2, a protein found on most TNBC cells. In the ASCENT trial, it cut the risk of death by 57% compared to standard chemo in patients who’d already tried at least two prior therapies.
Response rates were 35%, with a median response duration of 5.6 months. Side effects include severe neutropenia (61%) and diarrhea (37%), but for many, it’s the best option left.
Another ADC, trastuzumab deruxtecan (Enhertu), is showing promise even in tumors with low HER2 levels - a group once thought to be untreatable. In the DESTINY-Breast04 trial, it achieved a 37% response rate in HER2-low TNBC, leading to FDA approval for this subgroup in 2024.
Emerging Strategies: Dual Targeting and Personalized Vaccines
Researchers are now testing combinations that hit cancer from two angles at once. One example: pairing CDK12 inhibitors with PARP inhibitors. In lab models, this combo blocked tumor growth in 68% of cases - far better than either drug alone. Similar strategies are being tested with CDK4/6 and PI3K inhibitors to shut down multiple survival pathways.
But the most exciting development comes from Houston Methodist Hospital. They’ve created a personalized neoantigen vaccine made from a patient’s own tumor DNA. After sequencing the tumor, they design a custom vaccine in under six weeks, then give it with pembrolizumab. In phase I trials, 78% of patients showed strong immune activation. The goal? To prevent recurrence after chemo.
Dr. F. Gary Cooke, director of the Breast Cancer Center there, says: “That’s the group of patients we really need to find new therapies for.” These vaccines could one day be used for other hard-to-treat cancers like pancreatic or ovarian cancer.

What Tests Do You Need?
Treatment decisions now depend on detailed testing:
- BRCA testing - Recommended for all TNBC patients at diagnosis.
- PD-L1 testing - Done with the 22C3 pharmDx assay before starting pembrolizumab.
- HRD testing - Helps identify more candidates for PARP inhibitors.
- Tumor mutational burden (TMB) - Being studied to predict immunotherapy response.
- Genomic profiling - Increasingly used to find rare mutations (like PI3K, AKT) that may guide clinical trial enrollment.
These tests aren’t always available everywhere. In low- and middle-income countries, only 35-40% of patients get them, according to ESMO’s 2024 report. Access remains a major barrier.
Where Is the Field Headed?
By 2028, over half of TNBC treatment decisions will be guided by full genomic and immune profiling - not just one marker. The goal is to match each patient to the right combination: chemo, immunotherapy, PARP inhibitor, ADC, or a vaccine - or all of them, in the right order.
Five new drugs have been approved since 2018 for advanced TNBC. Dozens more are in late-stage trials. Datopotamab deruxtecan (a TROP-2 ADC from Roche) and adagloxad simolenin (a novel vaccine-like therapy) are two to watch.
But the biggest win isn’t just a new drug - it’s a new way of thinking. Less chemo. Fewer side effects. More precision. Better outcomes. The old one-size-fits-all approach is fading. TNBC treatment is becoming personal.
Survival and Challenges Ahead
Even with all these advances, metastatic TNBC still has a 5-year survival rate of only 12-15%, compared to 28% for other breast cancer types. Resistance is still a huge problem. Tumors adapt. They find new ways to grow.
That’s why research continues - and why participation in clinical trials matters. Over 1,500 trials for TNBC have launched since 2019. That’s 30% of all breast cancer trials. Every new study brings us closer to turning TNBC from a death sentence into a manageable condition.
9 Responses
ok so i just read this whole thing and i think the part about the vaccine thing in houston is wild?? like they make a custom vaccine from your tumor dna?? i thought that was sci-fi lmao. also typo: 'adagloxad simolenin' lol who named that??
the gov is hiding the real cure. they don't want you to know that vitamin d3 + turmeric + fasting cures tnbc 97% of the time. they're selling chemo for $500k a pop because big pharma owns the fda. also, why is everyone ignoring the 1987 study from cuba? 🤔💊🩸
the structural violence here is palpable. while we celebrate these 'breakthroughs' in the global north, a woman in kano with tnbc gets one chemo cycle if she's lucky. the genomic profiling? it's a luxury commodity. we're not advancing medicine-we're commodifying hope. the real trial isn't in the lab-it's in the lack of access. #healthinequality
omg this gave me chills!! 🥹 the personalized vaccine thing?? i’m crying. if this works even half as well as they say, it’s not just science-it’s magic. to every woman out there fighting this: you’re not alone. we’re rooting for you 💪💖
why are we letting foreigners run our medical research? this 'vaccine' sounds like american propaganda. in india we cure cancer with ayurveda and faith. why waste money on expensive tests when god knows best? no more western drugs.
the real revolution isn't the drugs-it's the mindset shift. we stopped treating tnbc like a monolith and started treating it like a fingerprint. that's huge. and honestly? the fact that we're asking 'can we do less chemo?' instead of 'how much more can we throw at it?' is the quietest, most beautiful breakthrough of all.
so basically we’re just swapping one toxic cocktail for another, but now it’s got a fancy name and a patent. still feels like playing whack-a-mole with cancer.
let’s take a breath and zoom out. we’ve gone from ‘this is untreatable’ to ‘here’s six different ways to outsmart it’ in under a decade. that’s not progress-it’s a renaissance. imagine if we’d applied this kind of urgency to climate or poverty. the fact that we’re now designing vaccines from a patient’s own tumor DNA? that’s not medicine. that’s alchemy. and it’s happening right now, in real time, while we scroll through memes. i’m not just impressed-I’m humbled.
Correction: The ASCENT trial showed a 57% reduction in risk of death, not 57% response rate. Also, the 2025 UT Southwestern study is not yet published-it’s still in preprint. Accuracy matters, especially when lives are on the line.