Tetracycline Sun Risk Calculator
Your Risk Level
Based on your inputs, you have a low risk of sun damage while taking tetracycline antibiotics.
Personalized Prevention Tips
What Is Tetracycline Photosensitivity?
You’re on tetracycline for acne, Lyme disease, or a respiratory infection, and suddenly your skin burns like you’ve been at the beach all day-even after just 20 minutes outside. That’s not bad luck. It’s tetracycline photosensitivity, a well-documented reaction where the antibiotic absorbs UV light and triggers skin damage. This isn’t rare. About 5 to 10% of people taking tetracycline-class drugs experience it, and for some, the reaction is severe enough to stop treatment entirely.
Unlike an allergic rash, this is phototoxic: the drug acts like a sponge for UV-A rays (320-425 nm), especially around 365 nm. Once activated, it creates reactive oxygen molecules that shred cell membranes, damage DNA, and inflame skin tissue. The result? Redness, blistering, peeling, and often dark, stubborn patches that linger for months. In 15-20% of cases, nails start lifting off the nail bed. Some even develop pseudoporphyria-fragile skin that blisters easily with minimal trauma, mimicking a rare genetic disorder.
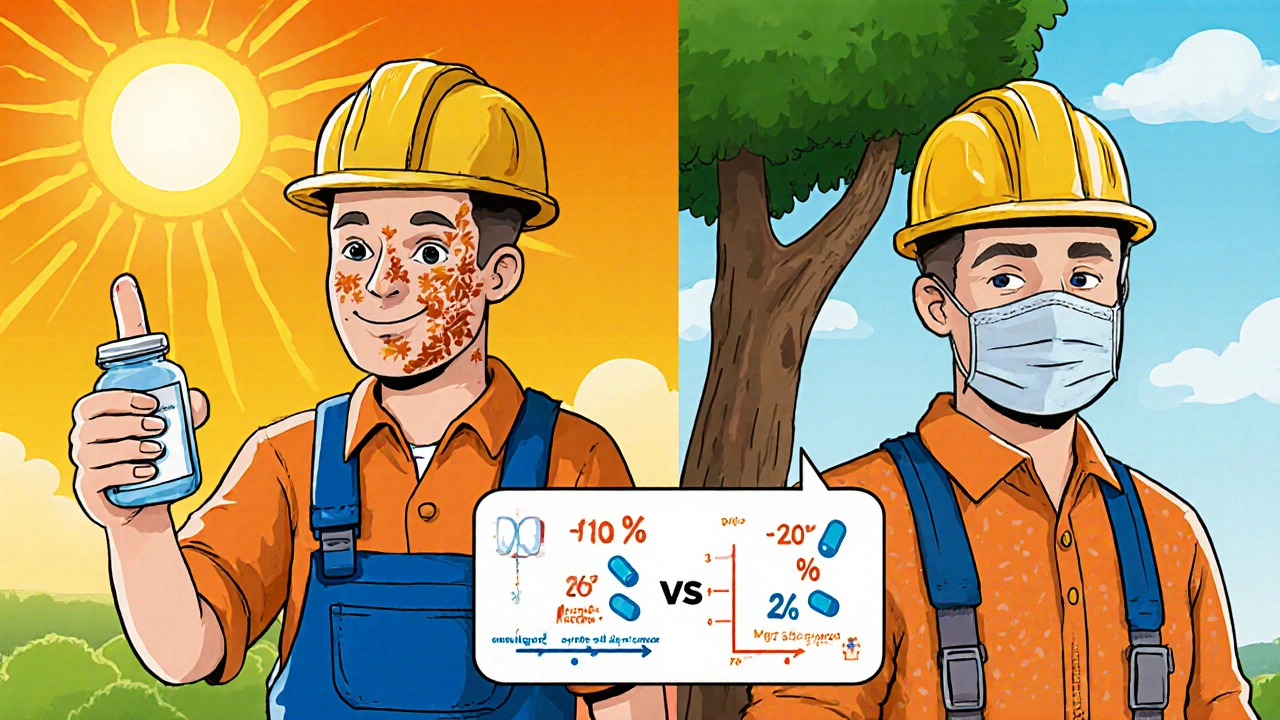
Not All Tetracyclines Are Equal
Just because you’re on a tetracycline doesn’t mean you’ll react the same way as someone else. The risk varies wildly depending on which drug you’re taking.
- Doxycycline is the biggest culprit. At 100 mg daily, about 15% of users get a reaction. At 200 mg, that jumps to over 40%. It’s the most prescribed tetracycline in the U.S.-and the most likely to cause sun damage.
- Demeclocycline is also high-risk, though less commonly used. It’s sometimes prescribed for SIADH, but its phototoxicity makes it a poor choice if you’re outdoors often.
- Tetracycline hydrochloride has moderate risk and is uniquely tied to pseudoporphyria cases.
- Minocycline is the safest option. Only 2% or fewer users report photosensitivity. It’s a top pick for acne patients who work outside or live in sunny climates.
- Sarecycline and omadacycline are newer derivatives designed to reduce this risk. Early data shows phototoxicity rates under 5%, but they cost 10-40 times more than generic doxycycline.
Why does this matter? If you’re on doxycycline for acne and spend even a little time in the sun, you’re at high risk. If you’re on minocycline, your odds drop dramatically-without losing much in effectiveness.
Who’s Most at Risk?
It’s not just about the drug. Your lifestyle, skin type, and environment play huge roles.
- People with fair skin burn faster and are more likely to develop lasting pigmentation.
- Outdoor workers-construction, farming, lifeguards, delivery drivers-get hit hardest. One study found 30% of outdoor workers on doxycycline developed noticeable reactions.
- Those in high-UV regions (Australia, Southern Europe, the Southwest U.S.) face 25-30% higher reaction rates than average.
- People who skip sunscreen or think “I’m just running to the car” won’t get burned. But UV-A rays penetrate clouds, windows, and light clothing. You don’t need to be at the beach to trigger this.
- Patients not warned by their doctor. A 2022 survey found 68% of people who had photosensitivity reactions said their provider never mentioned sun risk. That’s not negligence-it’s a systemic gap in education.
How to Prevent Sun Damage
Prevention isn’t complicated. It’s just consistent.
- Use mineral sunscreen daily. Chemical sunscreens (avobenzone, octinoxate) don’t block the full UV-A range that triggers tetracycline reactions. Stick to zinc oxide or titanium dioxide. Look for SPF 50+, broad-spectrum, and water-resistant. Apply 2 mg/cm²-that’s about a shot glass full for your whole body. Most people use less than half that.
- Avoid midday sun. UV-A is strongest between 10 a.m. and 4 p.m. Plan errands for early morning or late afternoon.
- Wear UPF 50+ clothing. Regular cotton offers barely any protection. Look for clothing labeled UPF 50+. A wide-brimmed hat cuts UV exposure to your face and neck by 73%.
- Use UV-blocking window film. Car windows block UV-B but let through 70-80% of UV-A. Installing film (available at auto shops) reduces exposure during commutes.
- Check your nails. If you notice one or more nails lifting from the bed after 3-6 weeks on tetracycline, talk to your doctor. Photo-onycholysis is common and often reversible if caught early.
- Don’t rely on “quick” protection. A 10-minute walk to the mailbox? Still enough. A lunch break outside? Still enough. This reaction doesn’t need sunburn levels of exposure.
What to Do If You Get a Reaction
If your skin turns red, swells, or blisters within hours of sun exposure while on tetracycline:
- Get out of the sun immediately.
- Cool the area with damp cloths-no ice, no butter, no aloe vera gel with alcohol.
- Take ibuprofen or acetaminophen for pain and inflammation.
- Don’t pop blisters. They protect the skin underneath.
- Call your prescriber. You may need to switch to minocycline or another antibiotic.
Dark spots from past reactions? They fade slowly, but can take 6-18 months. Topical retinoids or hydroquinone (prescription only) may help, but only after you’re off the antibiotic.
Alternatives to Tetracycline
If you’re constantly in the sun and need an antibiotic, there are other options.
- Minocycline is the top alternative for acne. Same effectiveness, much lower sun risk.
- Macrolides like azithromycin or clarithromycin work for respiratory and skin infections, though they’re not as broad-spectrum.
- Fluoroquinolones like ciprofloxacin carry their own phototoxic risk (5-7%), but newer ones like moxifloxacin are safer (<1% risk).
- Amoxicillin or cephalexin are good for many bacterial infections and don’t cause photosensitivity.
Switching isn’t always possible-doxycycline is the go-to for Lyme disease, Rocky Mountain spotted fever, and certain types of pneumonia. But if you’re on it for acne or rosacea, there’s a better option.
Why Doctors Still Prescribe It
Despite the risks, tetracyclines are still widely used because they work-especially doxycycline. It’s cheap, effective against MRSA, and treats a wide range of infections. In 2022, over 27 million prescriptions were filled in the U.S. alone. But the tide is turning. Dermatologists now prescribe minocycline for 65% of acne patients, while primary care doctors still reach for doxycycline 82% of the time.
Companies are responding too. Newer tetracyclines like sarecycline and omadacycline are designed to keep the benefits without the sun damage. Clinical trials show phototoxicity rates under 5%, and more are in development. But until they’re affordable, the choice comes down to cost versus safety.
Real Patient Stories
One Reddit user, u/SunSensitiveMD, a physician, shared: “I had three patients develop full nail separation on doxycycline 100 mg twice a day. All had to stop. None knew it could happen.”
Another patient on Healthgrades wrote: “I used doxycycline for rosacea for six months with zero issues. I wore SPF 50 every day, even indoors. No burns, no dark spots. It’s not hard-you just have to be consistent.”
But a RateMDs review says it all: “My dermatologist never mentioned the sun risk. I got a second-degree sunburn after 20 minutes at the beach on day three. I had to go to the ER.”
Final Takeaway
Tetracycline photosensitivity is preventable-but only if you know it’s a risk. It’s not a side effect you can ignore. It’s not something that only happens to people who sunbathe. It’s a direct chemical reaction that can happen during a walk, a drive, or even sitting by a window.
If you’re on tetracycline, ask: Which one? What’s my risk? Do I need to switch? And most importantly-am I protecting my skin every single day?
The answer could mean the difference between a minor burn and months of dark, lasting damage.

13 Responses
Just switched from doxycycline to minocycline last month and my skin hasn’t burned once. Seriously, if you’re outside at all, don’t risk it. My dermatologist didn’t even mention the sun thing until I showed up with a second-degree burn. Dumb oversight.
OMG YES I’VE BEEN THERE 😭 I thought I was just bad at sunscreen until I read this. Now I wear UPF shirts like they’re pajamas and my face looks normal for the first time in years. Also UV window film for my car? Genius. I’m buying it tomorrow.
This is the most life-saving post I’ve read since the Great Avocado Toast Rebellion of 2017. Tetracycline didn’t just ruin my tan-it ruined my confidence, my job interviews, my dating life. I now carry zinc oxide like it’s my emotional support weapon. Minocycline is my knight in shining armor.
It’s important to note that even on cloudy days, UV-A penetrates. Many patients assume they’re safe if it’s overcast, but that’s a dangerous misconception. Consistent protection is non-negotiable.
Minocycline isn’t safer. It’s just less documented. You’re still getting neurotoxicity and autoimmunity risks. This is just fearmongering dressed as advice.
Wait so if I take minocycline... can I still go to the beach? I really miss the beach.
Not if you’re not wearing a full-body wetsuit and a hat that blocks 99% of light. Even then, maybe just sip a coconut from under an umbrella. Trust me, your skin will thank you.
Ugh I hate how doctors just hand out antibiotics like candy and then act shocked when you turn into a lobster… I literally had to quit my outdoor job because of this… and now I’m broke AND scarred… #TetracyclineTrauma
Of course you got burned. You didn’t use SPF 100. You didn’t wear a face shield. You didn’t consult a photobiologist. This is why people die.
It should be emphasized that the phototoxic threshold for doxycycline is dose-dependent and cumulative. Daily exposure, even at low levels, results in subclinical cellular damage that may manifest as long-term dyspigmentation or premature aging.
Bro I took doxycycline in Arizona for two weeks. I came back looking like I’d been dipped in a lava lamp. My grandma cried. My dog avoided me. I now own three hats. One for each season. And a UV umbrella. It’s my new best friend.
As someone who works under the Nigerian sun daily, I can confirm this is real. I was on doxycycline for malaria prophylaxis and my arms looked like they’d been boiled. Switched to azithromycin and now I can walk to market without looking like a warning sign. Knowledge saves skin.
It is regrettable that the American medical establishment continues to prioritize cost-efficiency over patient safety. The widespread prescription of doxycycline without adequate patient counseling represents a systemic failure of ethical duty. This is not merely negligence-it is institutional abandonment.