Probiotic Timing Calculator for Antibiotic Therapy
To reduce antibiotic-associated diarrhea, take probiotics 2-3 hours after antibiotics. Enter the time you take your antibiotic dose below:
When you're on antibiotics, your body is fighting an infection-but it’s also quietly losing ground in your gut. Antibiotics don’t just kill bad bacteria. They wipe out the good ones too. And that’s when trouble starts: diarrhea, bloating, cramps, nausea. About 1 in 5 people on antibiotics get antibiotic-associated diarrhea (AAD). For some, it’s mild. For others, it’s a hospital-level complication called Clostridioides difficile infection (CDI), which can be life-threatening.
Why Antibiotics Mess With Your Gut
Your gut holds over 100 trillion bacteria. These aren’t just passengers-they’re essential workers. They help digest food, train your immune system, and keep harmful microbes in check. When you take antibiotics, it’s like sending in a bomb squad that doesn’t know the difference between criminals and civilians. Beneficial bacteria like Lactobacillus and Bifidobacterium get wiped out. Pathogens like C. diff move in fast, multiplying in the vacuum.What Probiotics Actually Do
Probiotics are live microbes-mostly bacteria or yeast-that can help restore balance. They’re not magic pills, but they’re one of the few tools with solid evidence behind them for reducing GI side effects. The most effective strains include Lactobacillus rhamnosus GG, Saccharomyces boulardii, and certain Bifidobacterium combinations. These strains don’t just replace lost bacteria. They produce acids that lower gut pH, block harmful bacteria from sticking to the gut lining, and even strengthen your intestinal barrier.The Evidence: Does It Work?
A major Cochrane review from 2020 analyzed 2454 people across 13 studies. The results were clear: in high-risk groups (like hospital patients), probiotics cut the chance of C. diff-associated diarrhea from 11.6% down to 3.1%. That’s a 70% drop. For general antibiotic diarrhea, probiotics reduced risk by about 50% in studies using S. boulardii and LGG. But not all probiotics are equal. A 2018 meta-analysis showed S. boulardii alone cut AAD risk by half. Other strains? Mixed results. Some combinations showed no benefit at all. This isn’t a one-size-fits-all fix. It’s strain-specific.Which Probiotics Actually Help?
Here’s what the data says works best for antibiotic use:| Strain | Reduction in AAD Risk | Dose Range (CFU/day) | Best Taken With |
|---|---|---|---|
| Lactobacillus rhamnosus GG | 50-60% | 5-10 billion | With food or 2 hours after antibiotic |
| Saccharomyces boulardii | 50% | 500-1000 mg (250-500 billion CFU) | On empty stomach |
| Bifidobacterium lactis BB-12 | 30-40% | 1-10 billion | With food |
| Multi-strain (LGG + B. lactis + others) | 40-50% | 10-20 billion | Varies by product |
Stick to these. Don’t waste money on random blends labeled “gut support.” Look for products that list the exact strain names and colony-forming units (CFUs). If the label says “probiotic blend” without specifics, skip it.
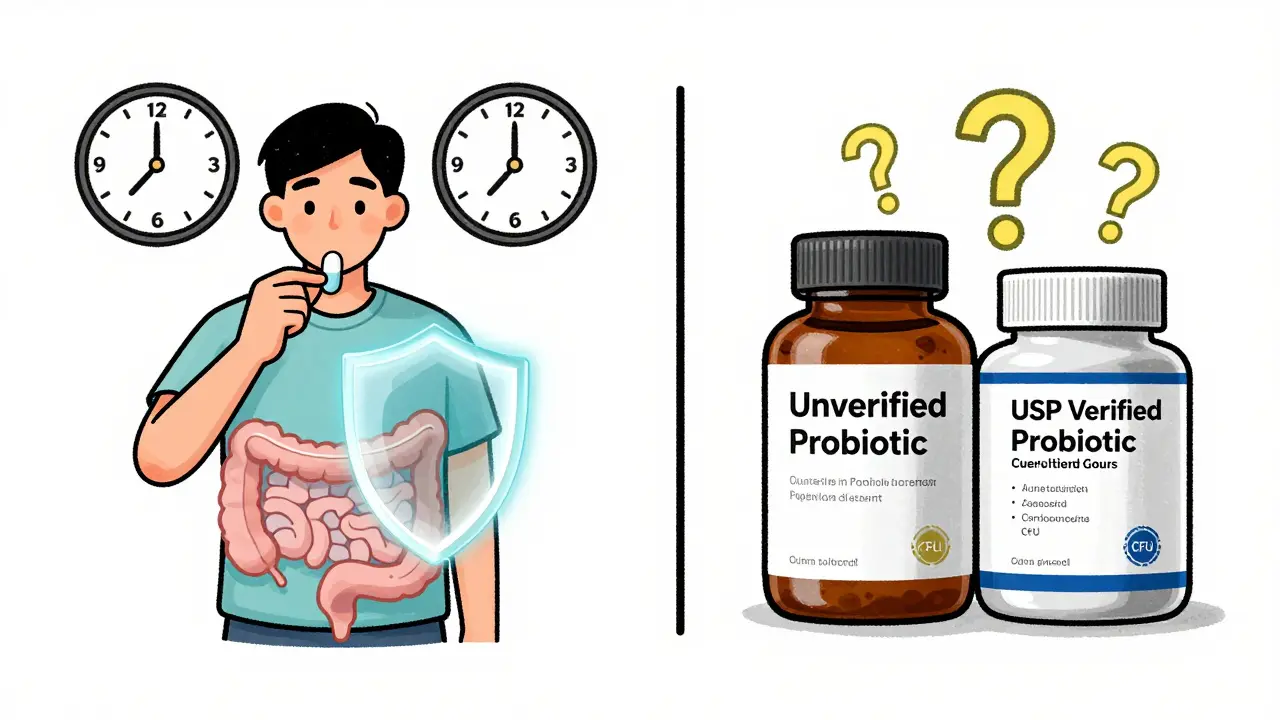
When and How to Take Them
Timing matters. Antibiotics can kill probiotics if they’re taken at the same time. The best practice? Space them out by 2-3 hours. Take your antibiotic in the morning, then your probiotic at lunch or dinner. Some experts suggest taking S. boulardii on an empty stomach since it’s yeast-based and acid-resistant. Lactobacillus strains often work better with food to protect them from stomach acid. Don’t stop after your antibiotic course ends. Keep taking probiotics for 1-2 weeks afterward. Your gut needs time to rebuild. Studies show people who stopped too early had higher relapse rates of diarrhea.Side Effects and Risks
Most people feel fine. But some report temporary bloating, gas, or constipation in the first few days. That’s normal. Your gut is adjusting. If it lasts longer than a week or gets worse, stop and talk to your doctor. Serious risks are rare-but real. There have been documented cases of bloodstream infections from Lactobacillus and fungal infections from S. boulardii, mostly in people with weakened immune systems, recent surgery, or central lines. If you’re on chemotherapy, have HIV, are recovering from major surgery, or are critically ill-do not take probiotics without your doctor’s approval.The Wild West of Probiotic Supplements
Here’s the ugly truth: most probiotics sold in the U.S. are classified as dietary supplements. That means the FDA doesn’t require manufacturers to prove they work-or even that they contain what’s on the label. ConsumerLab tested 50 popular probiotics in 2022. Thirty percent didn’t have the CFU count they claimed. Fifteen percent had extra microbes not listed-some potentially harmful. Amazon reviews for Culturelle (LGG) are glowing, with over 12,500 ratings averaging 4.2 stars. But that doesn’t mean every bottle you buy is the same. Look for third-party verified brands: USP, NSF, or ConsumerLab certified. These test for potency, purity, and label accuracy. Pay more? Yes. But it’s cheaper than a hospital visit for C. diff.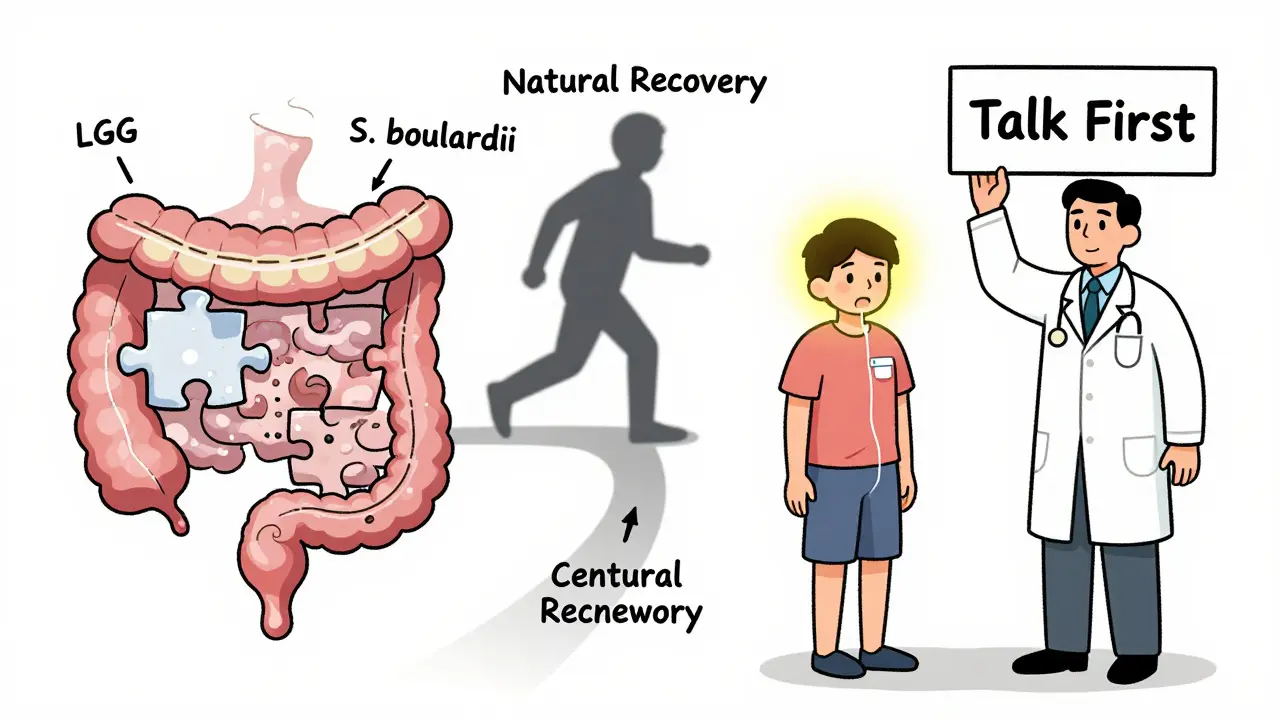
Food vs. Supplements
Yogurt, kefir, sauerkraut, and kimchi contain probiotics. But they’re not reliable for preventing AAD. The dose is too low, and strains vary. You’d need to eat 2-3 cups of yogurt daily to match a single supplement. Plus, many commercial yogurts are loaded with sugar, which can feed bad bacteria. Supplements give you precise strains and doses. For antibiotic use, supplements are the only practical option.Who Should Avoid Them?
Avoid probiotics if you:- Have a central line or catheter
- Are immunocompromised (cancer treatment, organ transplant, untreated HIV)
- Have short bowel syndrome
- Are critically ill or in ICU
- Have a history of endocarditis or bacterial infections from probiotics
If you’re unsure, ask your doctor. It’s not a risk worth guessing on.
What About Long-Term Gut Recovery?
Here’s the twist: a 2021 study in Nature found that taking probiotics after antibiotics might actually delay your natural microbiome recovery. People who took probiotics took months longer to return to their baseline gut bacteria than those who didn’t. The placebo group recovered faster because their own microbes rebounded naturally. So should you skip them? Not necessarily. For most people, preventing severe diarrhea is more urgent than perfect microbiome restoration. But if you’re healthy and just want to avoid mild bloating, you might not need them. The trade-off is real.What’s Next?
The FDA is working on new rules for live microbial products. A draft guidance came out in 2023, but it won’t be enforced until 2026 or later. Until then, the market stays unregulated. Meanwhile, researchers are studying personalized probiotics-matching strains to your specific antibiotic and gut profile. That’s the future. Right now, stick with proven strains, verified products, and good timing.Antibiotics save lives. But they come with a cost. Probiotics aren’t a cure-all-but for many, they’re the difference between a rough week and a dangerous complication. Choose wisely. Time them right. And always talk to your doctor before starting.
Can I take probiotics at the same time as antibiotics?
No. Antibiotics can kill probiotics if taken together. Space them out by 2-3 hours. Take your antibiotic first, then your probiotic later in the day. This gives the probiotic a better chance to survive and colonize your gut.
Which probiotic strain is best for antibiotic diarrhea?
The two most effective strains are Lactobacillus rhamnosus GG and Saccharomyces boulardii. Studies show they reduce diarrhea risk by about 50%. Avoid blends without these strains unless your doctor recommends one.
How long should I take probiotics after finishing antibiotics?
Continue for 1-2 weeks after your antibiotic course ends. Your gut needs time to rebuild its balance. Stopping too soon increases the chance of diarrhea returning.
Are probiotics safe for everyone?
No. Avoid probiotics if you’re immunocompromised, have a central line, are critically ill, or have recently had surgery. There’s a small but real risk of serious infection. Always check with your doctor first.
Do probiotics help with bloating and gas from antibiotics?
Yes. Many people report less bloating and cramping when taking the right probiotic strain. But some experience temporary increases in gas at first. That usually fades within a few days as your gut adjusts.
Can I get enough probiotics from yogurt instead of supplements?
Not reliably. Yogurt contains far fewer live cultures than supplements, and the strains aren’t always proven for AAD. You’d need to eat large amounts daily to match a single probiotic pill. Supplements offer precise, tested doses.
Are expensive probiotics better?
Not always. Price doesn’t equal quality. Look for third-party verification (USP, NSF, or ConsumerLab) instead. Many affordable brands meet standards. Avoid products that don’t list strain names and CFUs.
12 Responses
Oh wow, so now we're supposed to trust some random pill with 'probiotic' on it that's not even FDA-approved? 🤨 My cousin took one after antibiotics and ended up with a fungal infection-turns out the bottle had mold spores in it. And don't even get me started on how Big Pharma owns half these brands. They want you hooked on supplements so you never go back to eating real food. Also, why is Saccharomyces boulardii a yeast? Isn't that just a fungus? Like… are we feeding our guts mold now? 😬
Look, I get the appeal of a quick fix-pop a pill, fix your gut, boom, back to normal. But let’s not pretend this is science magic. The gut microbiome isn’t a Lego set where you swap out one block and everything clicks back into place. That 2021 Nature study? Yeah, it’s the elephant in the room. Probiotics might prevent diarrhea, sure-but they also delay natural recovery. So you’re trading a week of loose stools for months of your body playing catch-up. And if you’re gonna spend $30 on a bottle, at least make sure it’s not just sugar and glitter with a ‘live culture’ sticker slapped on it. Third-party verification? Non-negotiable. Otherwise, you’re just funding a wellness scam with your credit card.
This was so helpful. I was on antibiotics last winter and had awful bloating-I didn’t know probiotics could help. I just stuck with yogurt and felt worse. Now I’m going to get LGG with a USP seal. Thank you for breaking it down so clearly.
While the empirical evidence supporting the use of specific probiotic strains in mitigating antibiotic-associated diarrhea is indeed compelling, one must also acknowledge the methodological heterogeneity across the cited studies. The variability in dosage, timing, and strain composition introduces confounding factors that may limit generalizability. Furthermore, the absence of standardized regulatory oversight for dietary supplements necessitates a cautious approach, particularly in vulnerable populations. I would strongly recommend consultation with a clinical microbiologist or gastroenterologist prior to initiating any probiotic regimen.
Oh please. You’re telling people to take a pill that’s not regulated, from a company that doesn’t even know what’s in it, because some study says ‘it works’? That’s not medicine, that’s superstition. And don’t get me started on ‘Lactobacillus rhamnosus GG’-sounds like a pharmaceutical marketing department wrote it in a PowerPoint. Meanwhile, people are dying from probiotic sepsis, and you’re out here recommending it like it’s a vitamin. You think your gut’s a garden? It’s a battlefield. And you’re handing the enemy a grenade labeled ‘natural.’
Correction: The Cochrane review analyzed 2,454 participants across 13 RCTs-not ‘people.’ Also, ‘CFU/day’ is technically incorrect; it should be ‘colony-forming units per day.’ And you say ‘Saccharomyces boulardii’ is yeast-based-yes, but it’s a non-pathogenic, non-colonizing, transient yeast. Not a fungus in the mold sense. Also, your table mislabels the dose for S. boulardii: 500-1000 mg ≠ 250-500 billion CFU. That’s a 50x error. One milligram of S. boulardii ≈ 1 billion CFU. Fix your math. Or don’t. But then don’t pretend you’re giving medical advice.
Hey everyone-just wanted to say this post is a game-changer. I’ve been giving my grandma probiotics after her antibiotics for years, and she’s never had a stomach issue since. Seriously, if you’re on antibiotics, DO THIS. It’s not about being ‘perfect’-it’s about protecting yourself. I’m telling my whole family. And if you’re worried about cost? Look for sales on Amazon. I got a 3-month supply for $18 with USP certification. Small price to pay to not end up in the hospital. You got this 💪❤️
Let’s be real-this whole probiotic thing is a distraction. The real problem? Industrial food. Glyphosate. Fluoride in the water. The government doesn’t want you to heal naturally. They want you dependent on pills. Your gut isn’t broken because of antibiotics-it’s broken because of Monsanto, Big Pharma, and the FDA’s corruption. And now they’re selling you ‘Lactobacillus’ like it’s the answer? Wake up. The only real cure is fasting, raw vegetables, and drinking rainwater. Probiotics? Just another tool to keep you docile. They don’t want you strong. They want you buying bottles.
Interesting. But I wonder-what if the reason some people don’t recover naturally after antibiotics isn’t because they didn’t take probiotics, but because their microbiome was already compromised by years of processed food, stress, and sleep deprivation? Maybe the real issue isn’t the antibiotic, it’s the lifestyle. And if you’re relying on a pill to fix what your daily habits broke… that’s not a solution. That’s a Band-Aid on a broken leg.
Great breakdown. I especially appreciate the note about timing-so many people just take it all together and wonder why it doesn’t work. Also, the warning about immunocompromised individuals? Crucial. I’m a nurse, and I’ve seen too many cases where people self-prescribed probiotics and ended up in septic shock. Always check with your provider. This post saved someone’s life today.
While I appreciate the effort to synthesize the data, the article's presentation of the 2021 Nature study as a counterpoint to probiotic efficacy is misleading. The study did not conclude that probiotics 'delay recovery' universally-it demonstrated that certain strains may temporarily suppress endogenous microbiota repopulation in a subset of healthy adults. This is not equivalent to saying probiotics are harmful. Moreover, the authors themselves state that for high-risk patients, the benefits of preventing CDI far outweigh theoretical delays in microbial recovery. The conflation of correlation with causation here is concerning. Also: you wrote 'CFU/day'-it should be 'CFU per day.' And please, for the love of science, use proper capitalization.
As someone who grew up in Mexico eating fermented foods daily, I can say: your gut remembers. 🌮🌶️ My abuela never took probiotics-she ate nopal, kefir, and pickled jalapeños. But here’s the thing: she also never ate processed sugar or antibiotics unless absolutely necessary. Maybe the real ‘probiotic’ is a life lived with real food, not a pill from Amazon. Still, if you’re on antibiotics? Yeah, take the LGG. Just don’t forget to eat something alive after it. 🥬🧄✨