When your nose runs, your chest feels tight, or you wake up gasping at night because of allergies, you’re not just dealing with irritation-you’re dealing with inflammation triggered by chemicals called leukotrienes. These are not your typical allergens like pollen or pet dander. They’re internal messengers your body releases when it overreacts to triggers, causing airways to swell, tighten, and fill with mucus. That’s where montelukast comes in. Sold under the brand name Singulair and as generic tablets, chewables, and granules, montelukast is a leukotriene receptor antagonist. It doesn’t stop allergies from happening, but it blocks one of the worst parts of the reaction: the airway narrowing and swelling that makes breathing hard.
How Montelukast Actually Works
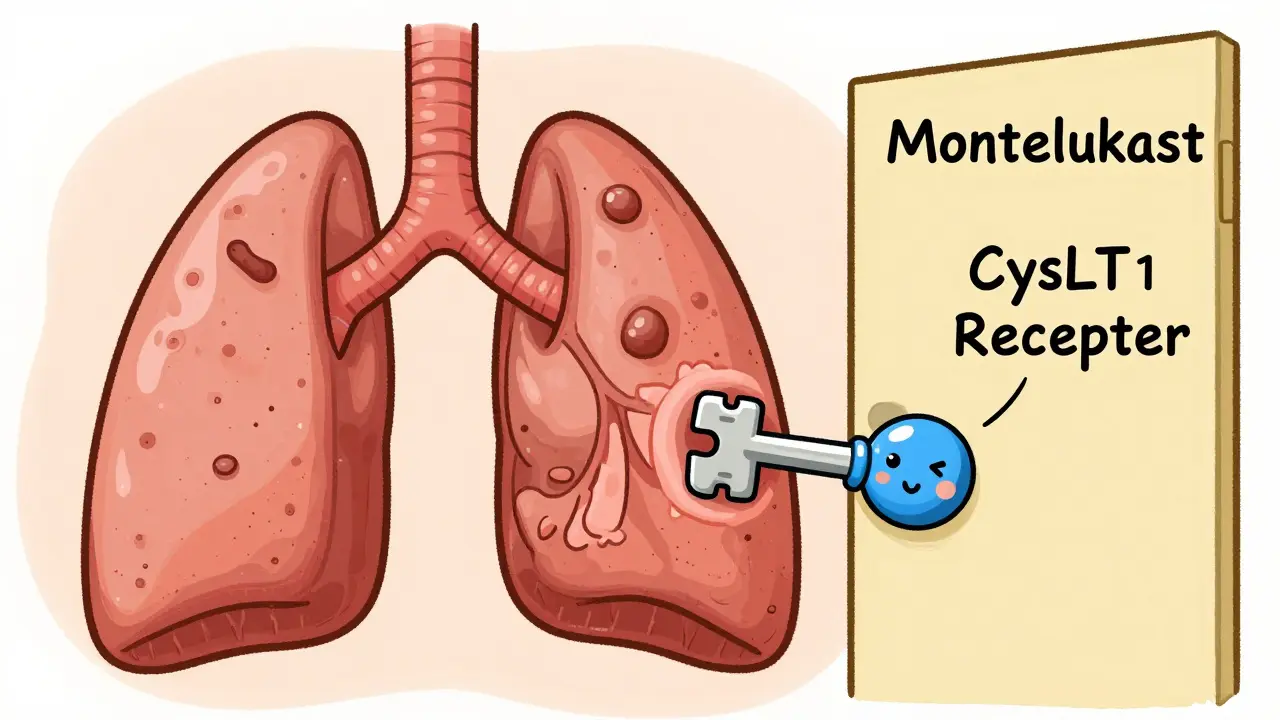
Montelukast works by locking onto a specific receptor in your lungs and nasal passages called CysLT1. This receptor is like a door that leukotrienes-LTC4, LTD4, LTE4-use to trigger inflammation. When these chemicals bind to the receptor, they cause airway muscles to contract, blood vessels to leak fluid, and mucus glands to go into overdrive. Montelukast steps in and blocks that door. It doesn’t reduce the amount of leukotrienes your body makes. Instead, it prevents them from activating their target. Think of it like putting a lock on a door so the intruder can’t get in, even if they’re still outside.
What makes montelukast special is its precision. Unlike older anti-inflammatory drugs that affect many systems in the body, montelukast is highly selective. It doesn’t interfere with beta-adrenergic receptors (which control breathing rate), cholinergic receptors (involved in mucus production), or prostanoid pathways (linked to pain and fever). This means it’s less likely to cause side effects like rapid heartbeat or dry mouth. Studies show that even a 5-milligram dose can block up to 75% of the bronchoconstriction caused by inhaled leukotrienes. That’s why it’s effective for both asthma and allergic rhinitis-it targets the same inflammatory pathway in both the upper and lower airways.
What Conditions Is It Used For?
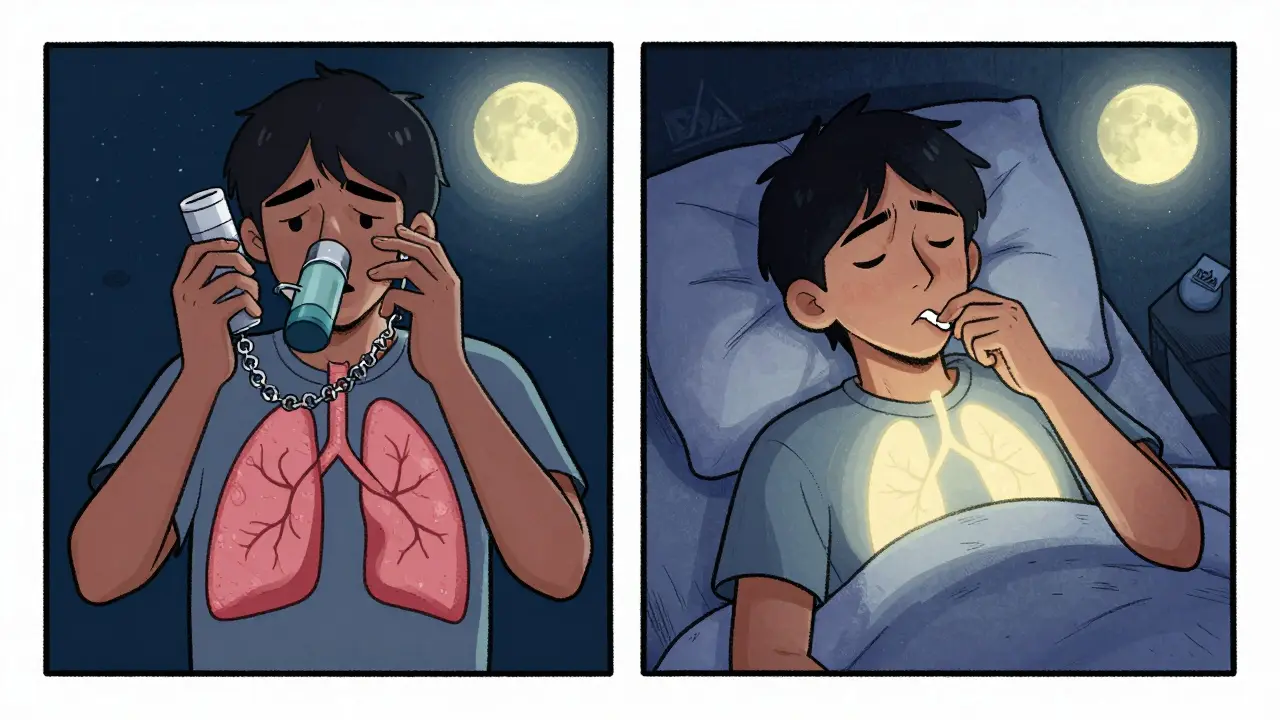
Montelukast is approved for two main uses: chronic asthma and allergic rhinitis. For asthma, it’s used for long-term control-not for sudden attacks. If you have mild to moderate persistent asthma, especially if you’re a child or someone who struggles with inhalers, montelukast can help reduce flare-ups, nighttime coughing, and reliance on rescue inhalers. In clinical trials, people taking montelukast used their albuterol inhalers 30-50% less often and saw measurable improvements in morning lung function.
For allergic rhinitis, whether it’s seasonal (hay fever) or year-round (from dust mites or pets), montelukast reduces nasal congestion, runny nose, and sneezing. It’s not as fast-acting as antihistamines like loratadine or cetirizine, but it works differently. While antihistamines block histamine-the chemical that causes itching and sneezing-montelukast blocks leukotrienes, which are the main drivers of nasal swelling and stuffiness. That’s why some people find it helpful when antihistamines don’t fully clear their congestion.
It’s also one of the few asthma medications approved for children as young as 12 months. The oral granule form can be mixed into applesauce or formula, making it one of the few options for toddlers who can’t use inhalers properly.
Where It Stands in Treatment Guidelines
Here’s the reality: montelukast is not the first choice. For asthma, inhaled corticosteroids (ICS) like fluticasone or budesonide are the gold standard. They reduce inflammation at the source and are far more effective at preventing severe attacks. For allergic rhinitis, second-generation antihistamines and intranasal corticosteroids are stronger and faster. So why does montelukast still get prescribed?
Because adherence matters. Many people-especially kids and busy adults-don’t use inhalers correctly. A study found that only 30-50% of children with asthma use their ICS inhaler as prescribed. Montelukast is a pill. One a day. No technique. No coordination. No spitting out medication because you didn’t inhale right. For those who can’t or won’t use inhalers, it’s a real alternative.
Guidelines from the Global Initiative for Asthma (GINA) and the American Academy of Pediatrics clearly state: ICS first. Montelukast second. But second doesn’t mean useless. It means “when first-line doesn’t work, isn’t tolerated, or isn’t feasible.” In fact, for patients with both asthma and allergic rhinitis, montelukast is one of the few drugs that treats both at once. That’s a big advantage over separate nasal sprays and inhalers.
Real-World Results: What Patients Actually Experience
People’s experiences with montelukast vary widely. Some report life-changing improvements. A parent on WebMD shared that after adding montelukast to her 6-year-old’s fluticasone inhaler, her daughter’s rescue inhaler use dropped from daily to once a week. Another user on Reddit said it eliminated their nighttime wheezing-something no antihistamine had done.
But others are disappointed. A 32-year-old woman on Drugs.com said it cut her allergy symptoms by about half but didn’t touch her nasal congestion like Zyrtec did. That’s consistent with the data: montelukast is less effective than antihistamines for sneezing and itching, but better for stuffiness. It also takes time. Unlike antihistamines that work in an hour, montelukast needs 24-48 hours to start working, and full benefit can take up to a week. If you expect instant relief, you’ll be let down.
And then there are the side effects. Most are mild: headache, stomach pain, cough. But some are more serious. In 2020, the FDA added a boxed warning about neuropsychiatric side effects-things like agitation, depression, nightmares, and suicidal thoughts. These are rare, but they’re real. A 2023 study in the Journal of Allergy and Clinical Immunology found that in patients with mastocytosis, montelukast helped reduce symptom frequency, but also noted that neuropsychiatric events were more common in teens and young adults. Doctors now screen patients for mood disorders before prescribing it.
How It Compares to Other Options
There are two other leukotriene modifiers: zafirlukast (Accolate) and zileuton (Zyflo). Zafirlukast works similarly to montelukast but needs to be taken twice daily and has more drug interactions. Zileuton blocks leukotriene production instead of blocking the receptor, but it requires liver monitoring and is taken four times a day. Montelukast wins on convenience: once daily, no blood tests, minimal interactions.
Compared to inhaled steroids, montelukast is less effective. One study showed ICS reduced asthma exacerbations by 50%, while montelukast reduced them by 20-30%. But montelukast has no steroid side effects-no voice hoarseness, oral thrush, or potential growth delay in kids. For families worried about long-term steroid use, that’s a big deal.
For allergic rhinitis, montelukast is weaker than nasal corticosteroids (like Flonase) and antihistamines (like Claritin). But if you’re already taking it for asthma, adding a nasal spray might be overkill. In those cases, montelukast alone can handle both conditions.
Who Benefits Most From It?
Montelukast isn’t for everyone. But it shines in specific situations:
- Children under 5 who can’t use inhalers properly
- Patients with both asthma and allergic rhinitis
- People who can’t tolerate or refuse inhaled corticosteroids
- Those with exercise-induced bronchoconstriction who don’t respond well to albuterol alone
- People who need a simple, once-daily regimen
It’s also a good option in low-resource settings. Generic montelukast costs $4-$10 a month. That’s cheaper than most nasal sprays and far less expensive than biologic injections for severe asthma, which can cost over $1,000 per dose.
What You Need to Know Before Taking It
If you’re considering montelukast, here’s what to remember:
- It’s not a rescue medication. Never use it during an asthma attack. Keep your albuterol inhaler handy.
- Take it every day, even if you feel fine. It works by preventing inflammation, not treating it after it starts.
- Take it in the evening. Some studies suggest nighttime dosing may improve asthma control, and it may help with sleep-related side effects.
- Watch for mood changes. If you or your child becomes unusually irritable, anxious, or has trouble sleeping, tell your doctor right away.
- Don’t stop it suddenly. If you need to discontinue, do it under medical supervision.
It’s not a magic bullet. But for the right person, it’s a quiet, reliable tool that keeps airways open without the hassle of inhalers or the side effects of steroids. It’s not the top choice-but for many, it’s the only choice that works.
Is montelukast safe for long-term use?
Yes, montelukast is considered safe for long-term use in most people. Clinical studies have tracked patients for up to 12 months without significant safety concerns beyond the known neuropsychiatric risks. The FDA and global health agencies continue to approve its use for chronic asthma and allergic rhinitis. Regular check-ins with your doctor are recommended, especially if you notice mood changes or sleep disturbances.
Can montelukast replace my inhaler?
No. Montelukast is a controller medication, not a rescue one. It won’t stop an asthma attack in progress. You still need a short-acting beta-agonist like albuterol for immediate relief. Even if montelukast improves your daily symptoms, you must keep your rescue inhaler on hand.
How long does it take for montelukast to work?
Some people notice improvement in symptoms within 24-48 hours, but it typically takes about a week to reach full effect. Unlike antihistamines that work fast, montelukast builds up its anti-inflammatory effect over time. Don’t stop taking it if you don’t feel better right away.
Does montelukast cause weight gain?
Weight gain is not a commonly reported side effect of montelukast. Unlike oral corticosteroids, which can increase appetite and fluid retention, montelukast doesn’t affect metabolism or hormones in a way that leads to weight gain. If you notice unexplained weight changes, other factors like diet, activity, or another medication may be involved.
Can I take montelukast with allergy pills like Zyrtec?
Yes. Montelukast can be safely combined with second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra). Since they work through different pathways-antihistamines block histamine, montelukast blocks leukotrienes-they can complement each other. Many patients with both asthma and allergic rhinitis take both for better overall control.
What’s Next for Leukotriene Inhibitors?
While newer biologics like dupilumab and omalizumab are changing the game for severe asthma, montelukast isn’t going away. Its low cost, simple dosing, and dual action on nose and lungs keep it relevant. For mild asthma, children, and people without access to expensive therapies, it remains a cornerstone. The future may see more research into its role in conditions like chronic sinusitis or mastocytosis, but for now, its job is clear: offer a safe, simple option for those who need it most-when the best option isn’t possible.
11 Responses
Montelukast is basically your body’s way of saying ‘I’m tired of fighting pollen’ and just locking the door on the chaos. It doesn’t stop the storm, but it stops the storm from knocking your walls down. Simple, elegant, and way underappreciated. I wish more people knew how much it helped my kid breathe at night without needing a nebulizer.
OMG YES I’VE BEEN ON THIS FOR 3 YEARS AND IT’S CHANGED MY LIFE 🙌 I used to wake up gasping every other night, now I sleep like a baby. Also no weird throat gunk like with inhalers. My allergist said it’s not ‘first-line’ but who cares when it works? 🤷♀️
They’re lying to you. Montelukast is a chemical trap set by Big Pharma to make you dependent. They know you won’t use inhalers so they push this pill that slowly messes with your brain. My cousin’s son started having nightmares after 2 weeks. They didn’t tell you that part, did they? 🚩
So it blocks the receptor but doesn’t reduce the leukotrienes so does that mean the body just keeps making more and more and eventually it stops working like antibiotics or is that not how it works
My 4yo takes this in applesauce and I cry every time I give it to her 😭 I used to spend nights rocking her in the ER now she runs around like a tornado with zero wheezing. Also I love that it’s cheaper than my coffee. ☕️❤️
Let’s be real - this drug is a Band-Aid on a bullet wound. Inhaled steroids are the only real solution. Montelukast is what you take when you’re too lazy or too incompetent to use an inhaler properly. It’s not a treatment, it’s a compromise. And yes, the neuropsychiatric risks are real. People die from depression masked as ‘bad sleep.’ Don’t romanticize mediocrity.
I’ve been on montelukast for my exercise-induced asthma and it’s been solid. Not perfect, but better than nothing. I take it with Zyrtec and it’s like having two different keys to the same lock. Works better together. No drama, no side effects. Just quiet relief.
Of course they push this pill - it’s cheaper than inhalers and you can’t return it. The FDA knew about the brain stuff for years but let it slide because it makes money. Also, why is it only approved for kids as young as 12 months? Who decided it was safe to chemically silence a toddler’s immune system? Someone’s got a bonus this quarter.
It is profoundly irresponsible to present montelukast as a viable alternative to inhaled corticosteroids without emphasizing the stark disparity in efficacy. The data is unequivocal: ICS reduces exacerbations by 50 percent; montelukast, a mere 20 to 30. To frame this as a ‘quiet, reliable tool’ is not only misleading, it is ethically negligent. Furthermore, the normalization of non-adherence as a justification for prescribing a less effective agent undermines the entire foundation of evidence-based medicine. We are not optimizing care - we are optimizing convenience, and the consequences for pediatric lung development are not yet fully understood. This is not a solution - it is a surrender.
USA spends billions on this junk while other countries just use saline rinses and air filters. Why are we medicating every sneeze? This pill is just another way to make people feel like they’re doing something when they’re really just avoiding the real fix - clean air, less pollution, and maybe not living next to a highway. Also, why is this so cheap? Because it’s barely doing anything.
So if i take this and zyrtec together does that mean im basically doing a full on allergy war with two different weapons?? Also my nose stopped running but now i have weird dreams about flying on a vacuum cleaner lmao