When you buy a pill, an inhaler, or a medical device, you assume it’s safe. But who makes sure it actually is? The answer lies in FDA inspection records-the behind-the-scenes audit trail that decides whether a factory gets to keep making medicine or gets shut down. For manufacturers, understanding what the FDA can and can’t see isn’t just about avoiding fines. It’s about survival.
What the FDA Can See During an Inspection
The FDA doesn’t walk into a factory and ask nicely. They show up with legal authority under Section 704(a)(1) of the Federal Food, Drug, and Cosmetic Act. Their checklist is brutal: production logs, batch records, equipment calibration data, validation reports, and any document tied to how a product was made. If it’s part of the Current Good Manufacturing Practice (CGMP) rules, it’s fair game.
What’s not? Internal quality assurance audits. That’s right. If your team runs a confidential audit to find problems before the FDA does, those reports are protected under Compliance Policy Guide (CPG) Sec. 130.300. This policy was designed to encourage honesty. Companies can admit mistakes internally without handing the FDA a roadmap of their worst failures.
But here’s the catch: if that same mistake leads to a product defect, investigation, or customer complaint, those records are no longer protected. The FDA demands them. And they’ll dig deep-into deviation reports, CAPA logs, and even employee interviews. The line isn’t blurry. It’s razor-thin.
What You Must Keep-and For How Long
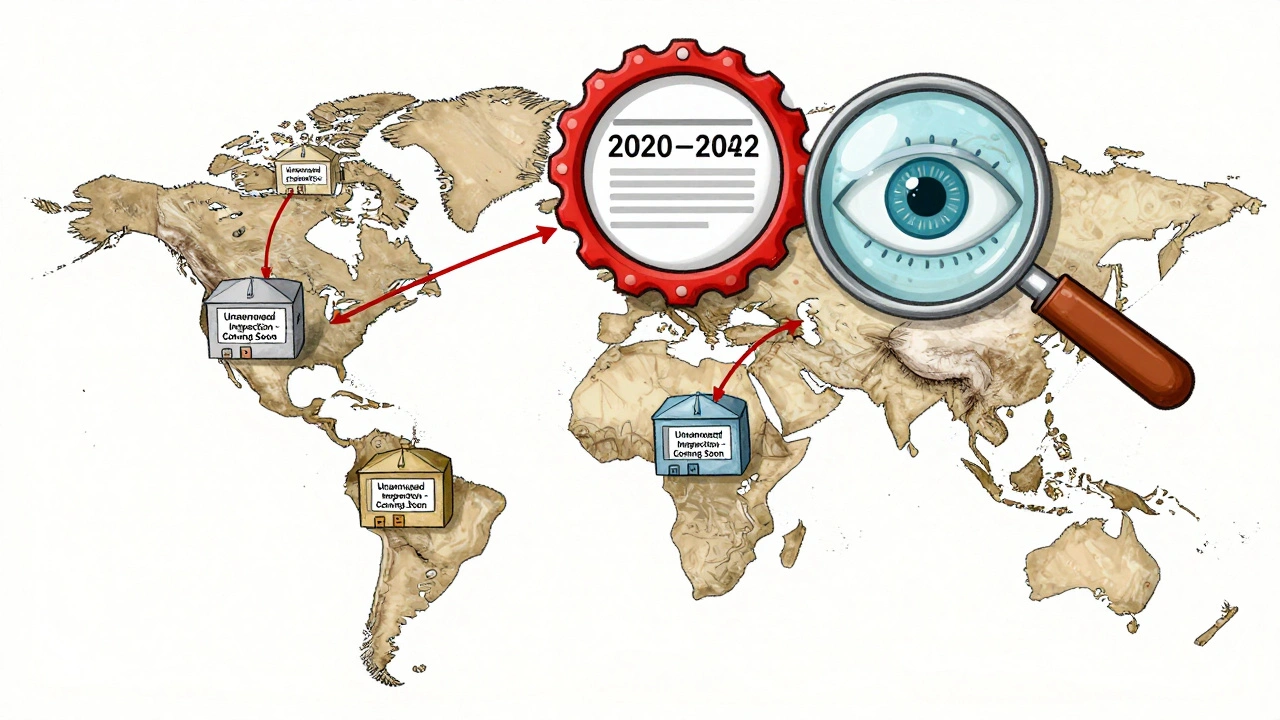
Record retention isn’t optional. It’s the law. For drug manufacturers, 21 CFR 211.180 says you must keep all CGMP records for at least one year after the product’s expiration date. For medical devices? 21 CFR 820.180 requires records to stay for the device’s entire lifespan plus two years. That means if you made a pacemaker in 2020, you’re still legally required to keep its manufacturing logs until 2042.
These aren’t dusty files in a basement. They need to be contemporaneous. That means records must be created in real time during production-not backfilled the next day. In 2024, 22% of FDA warning letters cited this exact violation. Companies that wait until after the fact to write down what happened? They’re already in trouble.
Form FDA 483: The Red Flag You Can’t Ignore
Every inspection ends with Form FDA 483. It’s not a suggestion. It’s a list of observations-things the inspector believes are out of compliance. You have exactly 15 business days to respond. Miss that deadline, and the FDA can escalate to a warning letter, import alert, or even a consent decree that shuts down your facility.
Responses matter. Companies that use FDA’s recommended root cause analysis method fix 89% of issues within six months. Those who rush with surface-level fixes? Only 62% resolve them. The difference isn’t luck. It’s discipline. A good response doesn’t just say, “We fixed it.” It explains why it happened, how you stopped it from recurring, and what you’re doing to prevent it next time.

Unannounced Inspections Are Now the Norm-Especially for Foreign Factories
In 2023, only 12% of foreign facility inspections were unannounced. By the end of 2025, that number will jump to 35%. The FDA is no longer waiting for a scheduled date. They’re showing up without warning to catch companies off guard.
Domestic facilities still mostly get scheduled visits-92% of the time, according to McGuireWoods’ 2025 analysis. But foreign manufacturers? They’re under siege. Why? Because the 2024 GAO Report found serious gaps in compliance overseas. The FDA’s message is clear: if you make medicine for Americans, you’re subject to the same standards-even if you’re halfway across the world.
Remote Regulatory Assessments: The New Normal
Since July 2025, the FDA has officially allowed Remote Regulatory Assessments (RRAs). This means they can ask for digital access to your systems-read-only views of your databases, video walkthroughs of your clean rooms, or electronic submission of records. No boots on the ground. Just a secure login.
RRAs aren’t inspections. They don’t generate Form 483s. But they’re becoming a gateway. If your digital records are messy, the FDA will likely follow up with a physical inspection. Companies using RRAs cut inspection-related downtime by 65%. That’s why 73% of Fortune 500 pharma firms have already built RRA-ready systems. If you haven’t, you’re falling behind.
Industry Pain Points: What Manufacturers Are Really Struggling With
On forums like Biophorum, quality managers are frustrated. One Merck QA manager said the 15-day response window for Form 483s is impossible during peak production seasons. Another from Pfizer admitted that 63% of their team over-disclose records-sending protected audit reports by accident-because the line between protected and required documents is confusing.
And it’s not just confusion. There’s inconsistency. A 2024 ECA Academy survey of 215 quality executives found that 41% got conflicting interpretations from different FDA district offices. One inspector says internal audits are off-limits. Another says they want them. That uncertainty forces companies to spend more on legal advice and compliance consultants.
On average, companies spend $385,000 a year just preparing for inspections. That’s training, documentation, software, and dedicated teams. And it’s growing. The global compliance market hit $12.7 billion in 2024-and it’s still rising.
How to Get Ready Before the FDA Shows Up
You don’t wait for the inspection to start training. You start months-or years-before. Here’s what works:
- Separate your documents. Keep internal QA audits in a locked folder labeled “Protected under CPG 130.300.” Everything else-deviations, complaints, CAPAs-goes in your CGMP system.
- Train your team. New hires need 6-9 months to understand the difference between protected and required records. Certification through RAPS boosts readiness by 37%.
- Automate where you can. Digital systems that timestamp entries, flag missing signatures, and auto-archive records reduce human error.
- Practice mock inspections. Run them quarterly. Bring in an outside auditor. See where your gaps are before the FDA does.
- Build an RRA-ready system. Even if you don’t think you’ll be asked, the FDA is moving fast. Your IT and quality teams need to be aligned.
The Bigger Picture: Is Transparency Working?
Between 2018 and 2022, 90.2% of pharmaceutical inspections found CGMP compliance. That sounds good. But behind those numbers are companies that slipped through. The FDA’s own Compliance Program Guidance Manual admits that protected audit reports can create “blind spots.”
Some experts, like former FDA Chief Counsel Daniel Troy, argue that hiding internal audits lets systemic problems fester. Others, like former Deputy Director Jane Axelrad, say it’s the only way to get honest feedback from employees. The truth? Both are right.
What’s clear is this: the FDA is moving toward more visibility, not less. The 2024 bipartisan Pharmaceutical Supply Chain Transparency Act proposed making some inspection findings public. The industry fought back, warning it would kill internal audits. But pressure is growing. The public wants to know where their medicine comes from.
Manufacturing transparency isn’t just about compliance. It’s about trust. The FDA doesn’t want to be the police. They want manufacturers to be the guardians of quality. And the only way that happens is if you’re ready-before they knock on your door.
Can the FDA see my internal quality audit reports?
Generally, no. Under FDA Compliance Policy Guide (CPG) Sec. 130.300, internal quality assurance audits conducted under a written program are protected from review during routine inspections. However, if those audits lead to a product deviation, complaint, or investigation, those specific records become accessible. The protection only applies to the audit report itself-not the underlying findings if they trigger a formal quality action.
What happens if I don’t respond to a Form FDA 483 within 15 days?
Missing the 15-day deadline for responding to a Form 483 almost always leads to a Warning Letter from the FDA. This is a formal enforcement action that can trigger import alerts, product seizures, or even consent decrees that shut down your facility. The FDA considers timely, thorough responses critical to resolving issues without escalation.
Are remote inspections replacing physical ones?
No-not yet. Remote Regulatory Assessments (RRAs) are supplemental tools, not replacements. As of mid-2025, RRAs accounted for only 8% of total inspections. They’re used to gather records or assess readiness before a physical inspection, but they cannot issue Form 483s. Physical inspections remain the primary enforcement mechanism, especially for foreign facilities and high-risk products.
How long do I need to keep manufacturing records?
For pharmaceuticals, you must keep CGMP records for at least one year after the product’s expiration date (21 CFR 211.180). For medical devices, records must be retained for the device’s entire lifespan plus two years (21 CFR 820.180). Records must be contemporaneous-created at the time of the activity-not backdated.
Why are unannounced inspections increasing for foreign facilities?
The 2024 GAO Report found significant compliance gaps in foreign manufacturing facilities supplying the U.S. market. To address this, the FDA increased unannounced inspections from 12% in 2023 to a target of 35% by the end of 2025. This shift is designed to catch facilities that might prepare only for scheduled visits, ensuring consistent quality standards regardless of location.

15 Responses
So the FDA can see everything except the stuff that actually matters? Classic. They want transparency but punish you for trying to fix things before they find out? Yeah right. This is just a tax on honest companies. Meanwhile, the big pharma giants with lobbyists are laughing all the way to the bank.
What if the real problem isn't the FDA, but the fact that we treat medicine like a product instead of a public good? We're outsourcing safety to bureaucrats who don't understand science, just paperwork. The system isn't broken-it was designed this way to protect profit, not people. Deep stuff, man.
US always thinks their rules are universal. In India, we don't have time for 15-day response windows. We fix it, or we don't make it. No fancy audits. No digital systems. Just people who care. Maybe you're overcomplicating survival.
lol anyone who thinks RRAs are legit is a sucker. The FDA can't even read their own emails, how they gonna review your database? And don't get me started on foreign factories-half of 'em are using Excel sheets from 2008. This whole transparency thing is just a scam to make consultants rich. #USAfirst
Internal audits are useless. If you need a report to find your own mistakes, you're already failing. Just fix the process. No paperwork. No delays. No drama. Simple.
Ohhhhh so now we’re supposed to bow down to FDA’s digital witch hunts?! Remote assessments?! That’s just corporate espionage with a badge! They want access to our systems like they’re some kind of tech-savvy CIA agent?! We’re not in a dystopian novel, people! This is a free country-wait, no it’s not anymore, is it?! #FDAOverreach #MakeMedicineGreatAgain
It is deeply concerning that the FDA permits the concealment of internal audit findings under the guise of 'compliance policy.' This undermines the very foundation of public health integrity. Such regulatory leniency is not only ethically indefensible-it is a gross dereliction of duty to the American citizenry.
Why do we keep pretending compliance is about safety and not about fear? The real question isn't what the FDA sees-it's who's scared of being caught. I've seen people cry over a missing signature. That's not quality control. That's trauma.
OMG I just read this and I’m crying 😭 Like, seriously-who thought this was a good idea?! The FDA is basically asking us to be both judge and jury AND therapist for our own mistakes?! And then they come in like, 'Oh, you didn’t fix it fast enough?' Ugh. I’m done. 🤦♀️💔 #ComplianceIsMental
Foreign factories getting unannounced inspections? That’s just colonialism with a badge. We don’t need FDA dictating how India or China runs their factories. They don’t even know what a monsoon is, how are they qualified to audit our pharma? This is about control, not safety.
Hey everyone, I just want to say-this stuff matters. I’ve seen families rely on these meds. I’ve seen workers stay up all night making sure every label’s right. This isn’t just paperwork. It’s people. So let’s not hate on the system. Let’s make it better together 💛
Actually, I think there's a deeper layer here that nobody's talking about-the psychological burden of constant compliance. It’s not just about the records or the inspections, it’s about the culture of surveillance that gets internalized. People start second-guessing every action, every decision, every signature. It creates a climate of anxiety that actually reduces innovation and makes people less likely to report problems because they fear punishment more than they fear failure. And that’s the real cost of this system, not the $385K per company-it’s the erosion of trust within the workforce itself. We need to ask: Are we building a culture of compliance, or a culture of fear?
So let me get this straight-you’re telling me the FDA can’t see your internal audits… but if someone complains about a pill, suddenly all bets are off? That’s not transparency. That’s a trap. And you’re telling me companies aren’t just lying to themselves to avoid getting caught? Please. This whole thing is a farce. The FDA doesn’t want clean factories-they want scapegoats.
Let me tell you something from Nigeria-we don’t have FDA inspectors. We have people who sell medicine on the street. If your pill doesn’t kill you in three days, you take another. This talk of ‘contemporaneous records’ and ‘RRA readiness’? It’s a luxury. The real problem isn’t compliance-it’s access. But you won’t hear that from the FDA, will you?
I just wanted to say how much I appreciate this breakdown. It’s so easy to feel overwhelmed by all the rules, but you made it feel human. I work in QA and sometimes I feel like I’m drowning in paperwork. But knowing that these systems exist to protect patients-it gives me purpose. Keep sharing this kind of stuff. We need more clarity, not more noise.