Starting a new medication can feel like a step forward in your health - until you realize you’re already taking five other pills, a handful of supplements, and that herbal tea your aunt swears by. Suddenly, what seemed simple turns into a minefield. Drug interactions aren’t rare. They’re common. And they can turn a helpful treatment into a dangerous one. The good news? You don’t have to guess your way through it. With the right steps, you can avoid serious side effects, hospital visits, and even life-threatening reactions.
Why Drug Interactions Happen
Not all medications play nice together. When two or more drugs are taken at the same time, one can change how the other works. This is called a drug-drug interaction. There are two main types: pharmacokinetic and pharmacodynamic.Pharmacokinetic interactions mess with how your body handles the drug - how it’s absorbed, broken down, or cleared out. The most common culprit? The liver enzyme CYP3A4. It processes about half of all prescription drugs. If one medication blocks this enzyme (like diltiazem or grapefruit juice), another drug can build up to dangerous levels. For example, taking simvastatin with diltiazem can raise simvastatin levels by over 300%, increasing the risk of muscle damage. That’s why doctors cap simvastatin at 10 mg per day if you’re on diltiazem.
Pharmacodynamic interactions are about what the drugs do to your body together. Take blood thinners, for example. Combining low molecular weight heparin with a direct oral anticoagulant (like apixaban) doesn’t just add up - it multiplies the bleeding risk by 300-400%. Or consider opioids and promethazine. Together, they can slow your breathing to a dangerous level - a combination that’s led to fatal overdoses.
High-Risk Combinations You Need to Know
Some interactions are so dangerous they’re listed in clinical guidelines as red flags. Here are a few you should never ignore:- Warfarin + Amiodarone: Amiodarone, used for heart rhythm problems, can make warfarin up to twice as potent. This can cause dangerous bleeding. Doctors typically cut the warfarin dose by 30-50% right after starting amiodarone and check your INR within 3-5 days.
- MAO inhibitors + Tyramine-rich foods: If you’re on phenelzine (Nardil) or other MAOIs, avoid aged cheeses, cured meats, and tap beer. Just one serving of blue cheese (with 2-5 mg of tyramine) can spike your blood pressure to over 200 mmHg - a medical emergency.
- St. John’s Wort + Antidepressants or birth control: This popular herbal supplement speeds up how fast your body breaks down drugs. It can drop cyclosporine levels by 40-60%, leading to organ rejection in transplant patients. It can also make birth control fail.
- Calcium channel blockers + Simvastatin: Amlodipine? Keep simvastatin at 20 mg max. Diltiazem or verapamil? Don’t go above 10 mg. Even small doses can cause rhabdomyolysis - a condition that breaks down muscle and can damage your kidneys.
These aren’t hypothetical risks. They’re documented in clinical studies and reported in real hospital cases. The American Academy of Family Physicians tracks these combinations because people get hurt - often because no one asked about supplements or over-the-counter meds.
What You Must Tell Your Doctor (Even If It Feels Unimportant)
Doctors don’t know what they don’t hear. Most medication reviews only list prescriptions. But nearly 70% of serious interactions involve something you bought without a prescription.Make a full list before your appointment. Include:
- All prescription drugs (even ones you take only once in a while)
- All supplements - vitamins, fish oil, magnesium, turmeric, melatonin
- Herbal remedies - St. John’s Wort, echinacea, garlic pills, ginkgo
- Over-the-counter painkillers - ibuprofen, naproxen, antacids with magnesium
- Alcohol and recreational drugs
Don’t downplay anything. A daily glass of wine? Important. Taking magnesium for leg cramps? Important. Using CBD oil? Very important. The American Heart Association found that 68% of patients never mention supplements - and that’s why interactions fly under the radar.
Pro tip: Take a photo of all your pill bottles or write down the names and doses. Don’t rely on memory. Your brain forgets. Your doctor won’t.
How to Spot Trouble Early
You don’t have to wait for a hospital visit to know something’s wrong. Watch for these signs in the first week after starting a new drug:- Unusual fatigue or weakness - especially if you’re on a statin
- Unexplained bruising or bleeding - gums, nose, cuts that won’t stop
- Confusion, dizziness, or extreme sleepiness - possible opioid or sedative buildup
- Swelling in ankles or rapid weight gain - could mean fluid retention from a blood pressure drug interaction
- Heart palpitations or chest tightness - especially if you’re on heart meds
If you notice any of these, don’t wait. Call your doctor or pharmacist. Don’t stop the medication unless told to - but don’t ignore it either. Early detection saves lives.
What Your Pharmacist Can Do That Your Doctor Might Not
Pharmacists are trained to catch interactions that slip past even experienced prescribers. At Mayo Clinic, pharmacist-led reviews cut hospital readmissions by 22% in just 18 months. Why? Because they do something most doctors don’t have time for: they look at everything.A pharmacist checks:
- Every prescription, OTC, and supplement
- How the drugs interact with your kidney and liver function
- Whether a cheaper or safer alternative exists
- Whether you’re taking the right dose at the right time
Ask your pharmacist to review your full list every time you get a new prescription. You don’t need an appointment - just walk in. Most community pharmacies offer this for free. And if you’re on five or more medications (which 45% of adults over 65 are), this isn’t optional - it’s essential.
When You’re Given a High-Risk Combination
Sometimes, your doctor has no choice. You need two drugs that interact. That doesn’t mean you’re out of options - it means you need a plan.Ask these four questions:
- Is there a safer alternative? For example, instead of simvastatin with amlodipine, ask about pravastatin - it doesn’t rely on CYP3A4 and won’t interact.
- Can the dose be lowered? Many interactions can be managed by reducing one drug’s dose. Simvastatin drops to 10 mg with diltiazem - and still works.
- Do I need extra monitoring? If you’re on warfarin and amiodarone, your INR needs checking every week for a month. Make sure you know when and where.
- What symptoms should I watch for? Get this in writing. Don’t just hear it - ask for a handout or email.
Don’t accept “it’s usually fine” as an answer. If a combination is high-risk, there’s a reason. Know the plan before you leave the office.
Technology Can Help - But Don’t Rely on It
Your EHR might pop up an alert when your doctor prescribes a new drug. But here’s the truth: doctors ignore 90-95% of these alerts. Why? Too many false alarms. Too much noise.High-severity alerts - like “contraindicated” or “50% dose reduction required” - get about 75% adherence. That’s better, but still not good enough. Don’t count on your system to save you.
Use free tools to double-check:
- DrugBank (free version available)
- MedlinePlus Drug Interactions Checker (from the NIH)
- Your pharmacy’s app - many let you upload all your meds and scan for conflicts
These aren’t perfect. But they’re better than nothing. And if you spot a warning, bring it up with your provider. You’re not overstepping - you’re protecting yourself.
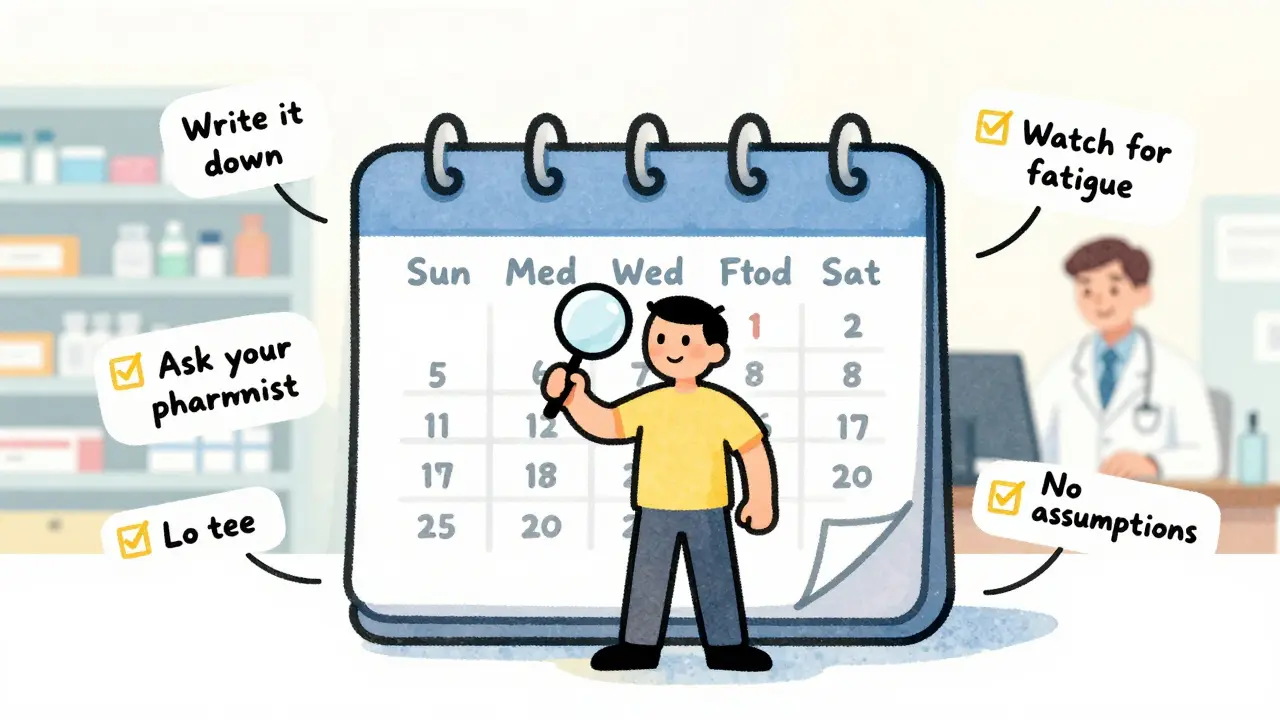
What to Do After Starting a New Medication
The first week is critical. Here’s your simple checklist:- Day 1: Take your first dose at home, not at work or out. Watch how you feel.
- Day 2-3: Check for side effects. Write them down.
- Day 5: Call your pharmacist or doctor if anything feels off - even if it seems minor.
- Day 7: Review your full med list again. Did you forget anything?
- Every 3 months: Schedule a medication review. Even if you feel fine.
Most people think once the new drug is started, they’re done. They’re not. Medication safety is ongoing. It’s not a one-time event - it’s a habit.
Final Thought: You’re the Most Important Person in This Equation
No doctor, pharmacist, or app can catch everything if you don’t speak up. You’re the only one who knows what you’re really taking - and how you’re feeling.Start today. Write down every pill, every supplement, every tea, every drink. Bring it to your next appointment. Ask your pharmacist to review it. Don’t wait until something goes wrong. The data is clear: 150,000 to 200,000 serious drug interaction events happen every year in the U.S. - and most are preventable.
Be the person who asks the questions. Be the one who writes it down. Be the one who doesn’t assume it’s fine.
Can I take over-the-counter painkillers with my new prescription?
It depends. Ibuprofen and naproxen can increase bleeding risk if you’re on blood thinners like warfarin or apixaban. They can also raise blood pressure if you’re on ACE inhibitors or beta-blockers. Acetaminophen (Tylenol) is usually safer, but it can harm your liver if you drink alcohol or take other liver-metabolized drugs. Always check with your pharmacist before taking any OTC painkiller.
Does grapefruit juice really interact with medications?
Yes - and it’s one of the most dangerous food-drug interactions. Grapefruit blocks CYP3A4, the enzyme that breaks down over 85 drugs. This includes statins like simvastatin, blood pressure meds like felodipine, and immunosuppressants like cyclosporine. Even one glass can raise drug levels by 300% and last over 24 hours. If you’re on any prescription, ask if grapefruit is safe - don’t assume it’s fine.
I take vitamins daily. Do they really interact with meds?
Absolutely. Vitamin K can make warfarin less effective. Calcium and iron can block absorption of thyroid meds like levothyroxine if taken at the same time. Magnesium can reduce the effect of antibiotics like ciprofloxacin. Even fish oil can thin your blood and increase bleeding risk with anticoagulants. Never assume vitamins are harmless - they’re active substances.
What if I forget to tell my doctor about a supplement I started last week?
Call your doctor or pharmacist as soon as you remember. Don’t wait for your next appointment. Many interactions happen within days of starting a new substance. It’s not embarrassing - it’s smart. Pharmacists see this every day. They’ve heard it all. The sooner you speak up, the sooner they can adjust your plan.
Are herbal remedies safer than prescription drugs?
No. Herbal products are not regulated like prescription drugs. St. John’s Wort, for example, can cut the effectiveness of birth control, antidepressants, and transplant meds by 40-60%. Garlic pills can thin your blood. Echinacea can interfere with immune drugs. Just because something is natural doesn’t mean it’s safe - especially when mixed with other medications.
How often should I review my medications?
Every 3 to 6 months, even if you feel fine. If you’re on five or more medications, aim for every 3 months. If you’ve had a hospital stay, surgery, or a new diagnosis, do it immediately. Your body changes. Your needs change. Your meds should too.
Next Steps: Your Action Plan
1. Make your list. Write down every medication, supplement, and OTC product you take - including frequency and dose. 2. Call your pharmacy. Ask for a free medication review. Bring your list. 3. Ask your doctor. “Is this new medication safe with everything else I’m taking?” Don’t let them brush you off. 4. Set a reminder. Schedule a medication review every 3 months. Put it in your calendar now. 5. Keep your list updated. Add new meds immediately. Remove ones you stop.Medication safety isn’t complicated. It’s just easy to forget. But when it matters - when your life could depend on it - you’ll be glad you didn’t.

12 Responses
I used to ignore my supplements until I ended up in the ER after mixing turmeric with warfarin. Don't be like me. Write it all down.
This is spot on. I'm a pharmacist and I see this every week. People think 'natural' means safe. Nope. St. John’s Wort messing with birth control? Happens more than you think. Always tell your pharmacist everything.
The CYP3A4 enzyme is the silent puppeteer of pharmacokinetics-its inhibition creates cascading dysregulatory phenomena that render polypharmacy a biochemically chaotic ballet. Grapefruit isn't just a fruit, it's a pharmacodynamic saboteur. We've normalized ignorance as convenience, and now we're paying the metabolic toll.
USA! USA! 🇺🇸 This is why we need better drug laws. Other countries don't let people just walk in and buy miracle herbs like it's a farmers market. My cousin took garlic pills with blood thinners and nearly died. We need to stop this madness.
i just wanna say i took my 10mg simvastatin with diltiazem for 6 months and nothing happened. maybe im just lucky? also i drink grapefruit juice every morning and my doc says its fine. idk. maybe the system is overreacting?
You got this. Small steps. Write it down. Call your pharmacist. You’re not being annoying-you’re being smart. Medication safety isn’t optional. It’s your right. Keep going.
I wish more people knew how powerful pharmacists are. I walked into my local pharmacy last month with a list of 14 things I was taking. They caught three dangerous interactions my doctor missed. Free service. Life-saving.
Interesting how this post assumes all patients are capable of maintaining a written log. What about the elderly with dementia? The low-income who can't afford to print or pay for apps? The non-English speakers? This advice is beautifully written, but deeply classist.
So let me get this straight... you're telling me I shouldn't drink grapefruit juice with my statin... but I can drink three beers and it's fine? Because alcohol is 'social' but citrus is 'dangerous'? What a joke.
Naija people know this! 🇳🇬 We don’t need no American doctors to tell us herbs don’t play nice with pills. My aunty took ginger + blood pressure med and her heart went boom-boom. Now she only takes her pills with water. No tea. No herb. No nonsense. Smart woman.
Just do it. Write it down. Call your pharmacist. It takes 10 minutes. You're not being a hassle-you're saving your life. Simple as that.
I started keeping a little notebook after my mom had a bad reaction. Now I update it every time I get a new script. I even take pics of the bottles. It’s weirdly comforting. Like I’m in control for once.