Why Your Insurance Might Reject Your Generic Medication Request
It’s not unusual to get a letter from your insurance company saying they won’t cover the brand-name drug your doctor prescribed. Instead, they want you to switch to a cheaper generic version. That’s normal-insurers do this to cut costs. But what if that generic won’t work for you? Maybe you had a bad reaction before. Maybe it doesn’t control your symptoms. Maybe your doctor says it’s unsafe. That’s when you need to appeal.
Insurance companies don’t just say "no" and walk away. They have a formal process called an appeal. And guess what? Most of them get overturned when done right. In fact, nearly 7 out of 10 appeals for generic medication denials succeed when the paperwork is solid. You’re not fighting a lost cause-you’re following a clear path.
Step 1: Understand the Denial Letter
Your denial letter isn’t just a rejection. It’s your roadmap. Every insurance company is required by law to explain why they denied your claim. Look for these key details:
- The exact name of the medication they denied
- The generic they’re pushing instead
- Whether it’s a step therapy issue (they want you to try cheaper drugs first)
- Whether it’s a prior authorization denial (they need more info before approving)
- The deadline to appeal-usually 180 days for private insurance
Don’t ignore this letter. If you toss it, you lose your right to fight. Save it. Highlight the denial reason. Write down the date you got it. That’s your starting line.
Step 2: Get Your Doctor on Board
You can’t win this alone. Your doctor is your most powerful ally. Insurance companies don’t care what you think-they care what your doctor says. Ask them to write a letter of medical necessity. This isn’t just a note. It needs to include:
- Why the brand-name drug is medically necessary (not just "I prefer it")
- Proof you tried and failed the generic or other alternatives
- Specific side effects you experienced with the generic
- References to clinical guidelines (like those from the American College of Physicians or specialty societies)
Doctors who include these three things have a 75%+ success rate, according to healthcare attorneys. If your doctor says they’re too busy, offer to draft it for them. Most will sign it if the facts are clear.
Step 3: Fill Out the Official Appeal Form
Every insurer has a form. Some call it a "Prior Authorization Exception Request." Others call it a "Step Therapy Override." Don’t guess. Call your insurer or log into your member portal and download the exact form. Fill it out completely. Miss one box, and they can deny you on a technicality.
Attach your doctor’s letter. Include your name, policy number, date of denial, and the medication details exactly as they appear on the denial letter. Don’t skip the part asking for clinical justification. That’s where your doctor’s letter does the heavy lifting.
Step 4: Submit Everything-And Keep Proof
Don’t just email it. Don’t just drop it in the mail. Use certified mail with return receipt, or submit it through your insurer’s secure online portal with a confirmation number. Keep a copy of everything: the form, the letter, the denial letter, your submission receipt. If you call them later to check status, you’ll need these.
Insurers have 30 days to respond if you haven’t started the medication yet. If you’re already taking it, they have 60 days. For urgent cases-like if you’re at risk of hospitalization-you can request an expedited review. That cuts the timeline to 4 business days. Make sure you mark your request as "urgent" and explain why.

Step 5: If They Say No Again, Go Higher
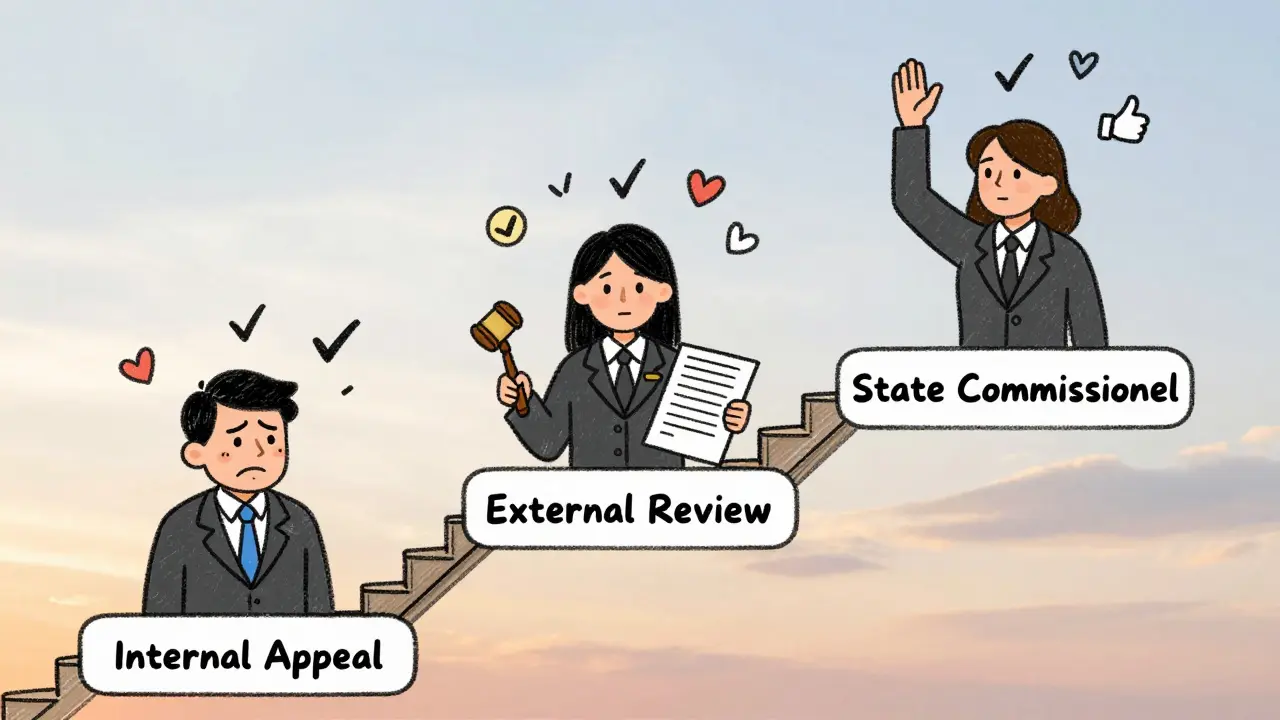
Most appeals get denied the first time-even if they’re valid. That’s why there’s an external review. If your internal appeal fails, you can ask for an independent third party to review your case. This is where things get serious.
For private insurance, this step is mandatory. The insurer must tell you how to request it in your denial letter. For Medicare Part D, you move to Level 2: Independent Review Entity. This is where the most appeals get overturned-63% of them, according to CMS data.
At this stage, you can submit new evidence. Maybe your doctor adds lab results. Maybe you include a case study from a medical journal. The reviewer isn’t tied to your insurer. They’re supposed to be neutral. Use this chance to strengthen your case.
Step 6: Involve Your State Insurance Commissioner
If you’ve gone through both levels and still got denied, your next move is your state’s insurance department. Every state has one. In California, they resolve 92% of formal complaints within 30 days. In New York, they require peer-to-peer reviews within 72 hours.
Call them. File a complaint. Be clear: "I’ve exhausted all internal and external appeal options, and I still can’t get my prescribed medication." They don’t have the power to force the insurer to approve it-but they can pressure them. And insurers hate that.
What Makes Appeals Fail (And How to Avoid It)
Most failed appeals have the same problems:
- No doctor’s letter
- Letter is too vague: "I think this drug is better" instead of "Patient had severe nausea and vomiting with generic metformin, confirmed by lab values on 3 occasions"
- Missing documentation of prior treatment failures
- Missing the deadline
- Not marking the request as urgent when it’s urgent
Patients who use a template from the Crohn’s & Colitis Foundation or Patient Advocate Foundation have a 65% success rate. Those who wing it? Only 32%. Don’t be the person who loses because they didn’t use a checklist.
How Long Does This Really Take?
Real talk: It’s not fast. The average appeal takes 52 days from start to finish. Some take longer. Some get approved in 10 days. It depends on your insurer, your doctor’s responsiveness, and whether you requested an expedited review.
Medicare appeals can drag out because they have five levels. But if you’re in a crisis, you can skip steps. Just say so in writing.
Track every date. Set reminders. If you haven’t heard back in 45 days, call. Ask for a case number. Ask who’s handling it. Keep pushing. Insurance companies count on you giving up.
Success Stories: Real People, Real Wins
A Type 1 diabetic in Ohio was denied semaglutide because her insurer wanted her to try cheaper insulin first. She had severe hypoglycemic episodes with every alternative. Her doctor documented every low-blood-sugar event over six months. The appeal was approved on the second level. She’s now stable.
A woman in Texas with rheumatoid arthritis was told to switch from a brand-name biologic to a generic. She developed a rash and joint flare-ups within days. Her rheumatologist submitted photos, lab results, and a letter citing the American College of Rheumatology guidelines. Approved on first appeal.
These aren’t rare. They’re routine-for people who know how to fight.
What’s Changing in 2026?
The Biden administration is pushing to cut Medicare Part D appeal times from 7 days to 3 for urgent cases. California’s new rule requires insurers to respond to step therapy exceptions within 48 hours if clinical documentation is clear. Digital platforms are rolling out across insurers-some already cut approval times by 40%.
But the core hasn’t changed: your doctor’s words, backed by facts, still win the day.
Final Tip: Don’t Wait Until You’re Out of Medicine
If you’re running low, don’t wait until your last pill to start the appeal. Start now. Even if you’re just thinking about it. The clock starts ticking the day you get that denial letter. And your health can’t wait.
Can I appeal if my insurance denies coverage for a generic medication I’ve never taken?
Yes. Even if you haven’t tried the generic, your doctor can still argue it’s unsafe for you based on your medical history-like allergies, past reactions to similar drugs, or conditions that make generics less effective. Documentation of clinical guidelines and physician judgment is enough to start the appeal.
How much does it cost to appeal an insurance denial?
Nothing. By federal law, insurance appeals are free. You can’t be charged for filing an internal or external appeal. Some patient advocacy groups offer free help with forms, but you don’t need to pay anyone to submit your appeal.
What if my doctor won’t help me appeal?
Try another provider. Many doctors will write the letter if you bring them a template. You can find free templates from the Crohn’s & Colitis Foundation or the Patient Advocate Foundation. If your doctor refuses, ask for a referral to another provider who’s willing to support your case.
Can I appeal for multiple medications at once?
Yes. You can submit one appeal covering multiple drugs if they’re all being denied under the same policy rule-like step therapy for all your chronic condition meds. Just list each one clearly and explain why each one needs an exception. Bundling saves time and shows a pattern.
Will my insurance raise my premiums if I appeal?
No. It’s illegal for insurers to retaliate against you for filing an appeal. Your rates can’t change based on whether you appeal or win. The law protects you from this kind of discrimination.
Next Steps: What to Do Right Now
1. Find your denial letter. If you can’t find it, call your insurer and ask for a copy.
2. Call your doctor’s office. Ask if they can write a letter of medical necessity. If yes, ask when they can get it done.
3. Download your insurer’s appeal form. Look on their website under "Member Services" or "Prescription Drug Appeals."
4. Set a reminder for 30 days from today. If you haven’t heard back by then, call again.
You’ve got this. Thousands do it every month. You just need the right documents-and the will to follow through.

12 Responses
This whole guide is just a scam to make doctors do free paperwork. Insurance companies know you’ll give up after the third form. I’ve been through this three times-each time they approved it on the 45th day, right when I was about to stop taking the meds. Lazy. Just lazy.
There’s a deeper philosophical tension here between corporate efficiency and individual biological uniqueness. The system is engineered to minimize cost, not maximize health-and yet, we’re expected to navigate it like a maze designed by someone who hates us. The doctor’s letter isn’t just paperwork; it’s a linguistic act of resistance. A handwritten testament to the fact that biology refuses to be standardized. And still, we’re told to be grateful for the generic. As if our bodies were interchangeable widgets on an assembly line.
I had to appeal for my dad’s blood pressure med last year. Doctor wrote the letter, I sent it certified mail, and they approved it in 11 days. No drama. Just follow the steps. You got this. 💪
Stop overcomplicating it. Get the letter. Send it. Done.
so like… if your doc is lazy and you dont wanna deal with the form… can you just like… buy the brand name? like off the internet? idk. i think the system is rigged. but also… why do we even have generics if they dont work? capitalism.
Appeals? How quaint. In India we just pay out of pocket. Insurance is a Western illusion. You think bureaucracy solves health? No. Money does. And if you can't afford the brand, maybe you shouldn't be on it.
I just want to say-thank you for writing this with such clarity and compassion! So many people feel lost in this process, and you’ve given them a map! I’ve shared this with my support group, and everyone’s been so grateful! Please keep doing this kind of work-you’re making a real difference!
Why do Americans always cry about insurance? In my country we don’t have this nonsense. You want the drug? Pay for it. If you can’t afford it, you’re not entitled to it. This whole appeal thing is just entitlement culture wrapped in a lab coat. And don’t even get me started on the ‘doctor’s letter’-like, who gave them the authority to play god?
Thank you for this. I’m a nurse in rural Ohio, and I see this every week. People are terrified to fight back. I always print out your steps and hand them out. One woman cried when she got approved-said she’d been skipping doses to make it last. You’re helping people live. That’s huge.
Lmao I tried this last year for my RA med. Doctor said ‘nah, I don’t have time.’ So I drafted the whole thing myself in Google Docs, sent it to him, he signed it in 2 minutes. Insurance denied. Then I called them back and said ‘I’ve got a letter from my rheumatologist, the FDA, and my therapist who says this med is keeping me from suicide.’ They approved it next day. Moral? You gotta be loud. And weird. And unapologetic. Also, I’m from India, and yeah, we don’t have this crap-but I’m glad we do, because it means we get to fight for our lives. So fight.
Has anyone tried appealing for a generic that’s not bioequivalent? Like, the actual active ingredient is the same but the fillers are different and cause migraines? Is that even considered a valid medical reason? I’ve got a whole journal of symptoms…
OMG I can’t believe you’re still letting insurance control your life 😭 Like, have you tried asking your doctor for a different brand? Or switching to CBD? Or just… not being so weak? This is why America is falling apart. You’re all so entitled. 😒