Sleep-Pain Cycle Assessment Tool
How Much Does Poor Sleep Affect Your Pain?
Answer these questions to assess your personal insomnia-pain cycle and get tailored advice.
Your Assessment Results
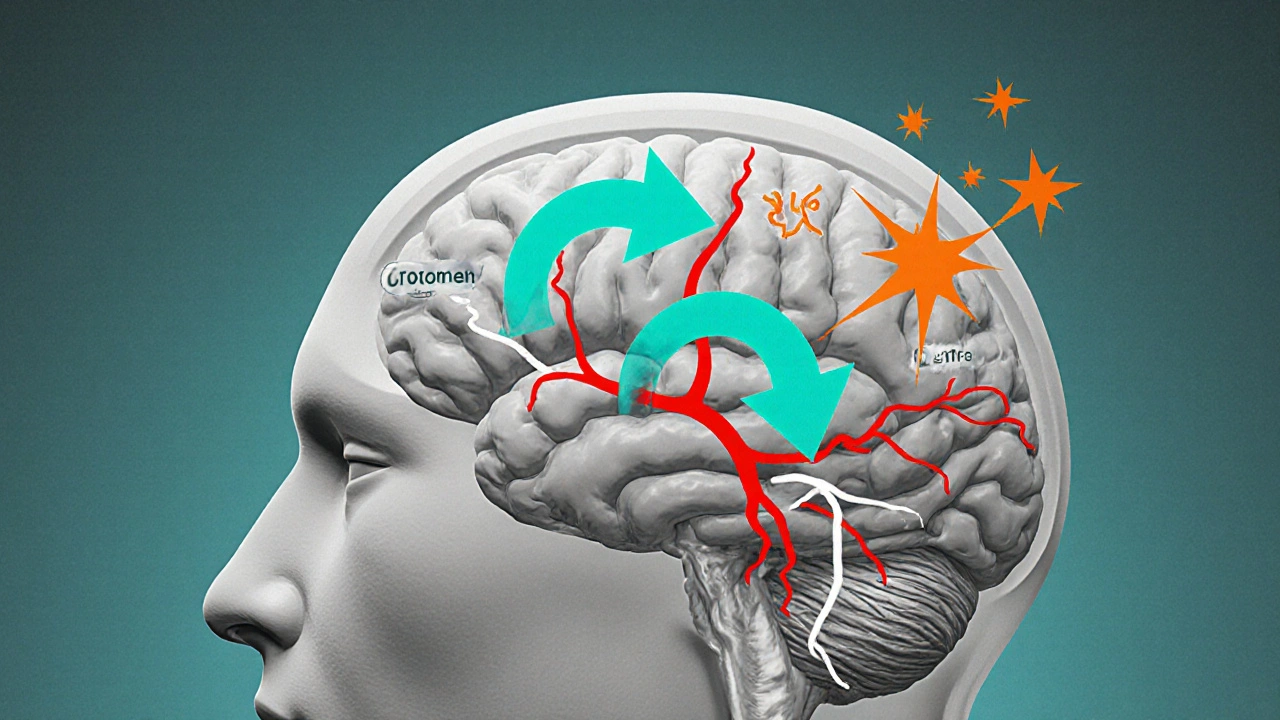
Ever wondered why a restless night seems to make yesterday’s aches feel brand new? The link between insomnia and chronic pain isn’t just a coincidence-poor sleep can actually turn up the volume on pain signals, while lingering pain can keep you tossing and turning. Below we break down the science, show how the cycle starts, and give you practical steps to break it.
What Is Insomnia?
Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, or achieving restorative sleep despite adequate opportunity. It affects roughly 10‑15% of adults in the United States and is linked to daytime fatigue, mood swings, and reduced cognitive performance. The condition can be acute (lasting days to weeks) or chronic (persisting three months or longer).
Understanding Chronic Pain
Chronic Pain refers to persistent pain that lasts longer than the usual healing time, typically over three months. Conditions such as arthritis, fibromyalgia, lower back disorders, and neuropathy fall under this umbrella. Chronic pain isn’t just a symptom; it’s a complex condition involving nervous system changes, emotional factors, and often, ongoing inflammation.
How Sleep Deprivation Alters the Body’s Pain Pathways
When you don’t get enough quality sleep, several biological systems tip over, creating a fertile ground for heightened pain.
- Sleep Architecture is the structure of sleep stages (light, deep, REM). Insomnia truncates deep‑stage sleep, which is when the body releases growth hormone and performs cellular repair. Missing this stage reduces tissue recovery and leaves muscles and joints more vulnerable.
- Inflammation rises after sleep loss. Pro‑inflammatory cytokines such as interleukin‑6 (IL‑6) and tumor necrosis factor‑alpha (TNF‑α) increase, amplifying pain signals in the peripheral nerves.
- Cortisol is the primary stress hormone. Sleep deprivation spikes cortisol levels, which can sensitize nociceptors (pain receptors) and impair the brain’s ability to dampen pain.
- Neurotransmitters such as serotonin and dopamine become imbalanced. Low serotonin reduces the brain’s natural analgesic pathways, making pain feel sharper.
In short, a night of poor sleep rewires the nervous system to over‑react to everyday aches.
How Chronic Pain Disrupts Sleep
It’s not a one‑way street. Persistent pain feeds back into sleep quality, creating a vicious loop.
- Physical discomfort makes it hard to find a comfortable position, leading to frequent awakenings.
- Pain‑related anxiety raises heart rate and breathing, keeping the brain in a heightened alert state.
- Some pain medications, especially opioids, can alter sleep architecture by suppressing REM sleep, while NSAIDs may cause gastrointestinal discomfort that awakens you.
The result? Even if you manage to get a full 8‑hour window, the sleep you achieve often lacks the deep, restorative stages your body needs.
Breaking the Cycle: Evidence‑Based Strategies
Addressing both sides of the loop yields the best relief. Below are interventions that target sleep, pain, or both.
| Intervention | Primary Target | Typical Benefits | Key Considerations |
|---|---|---|---|
| Cognitive Behavioral Therapy for Insomnia (CBT‑I) | Sleep behavior & thoughts | Improves sleep latency, reduces wake after sleep onset | Requires 6‑8 weekly sessions; limited by therapist availability |
| Melatonin Supplementation | Circadian regulation | Helps reset sleep‑wake cycle; modest pain‑modulating effect | Best for shift‑workers or jet‑lag; dosage 0.5‑5mg |
| Physical Exercise (Low‑Impact Aerobics) | Musculoskeletal health | Reduces inflammatory markers, improves sleep depth | Consistency matters; avoid intense workouts close to bedtime |
| Acetaminophen / NSAIDs | Pain relief | Quick reduction of inflammation‑related pain | Long‑term GI risk; may interfere with sleep if taken late |
| Mindfulness‑Based Stress Reduction (MBSR) | Stress & pain perception | Lowers cortisol, improves pain tolerance, enhances sleep quality | Requires regular practice; benefits emerge after weeks |
Below are actionable steps you can start today.
- Set a consistent sleep schedule. Go to bed and wake up at the same time, even on weekends. This stabilizes circadian rhythm and reduces cortisol spikes.
- Optimize your bedroom. Keep the room cool (≈65°F), dark, and quiet. Use blackout curtains or a white‑noise machine to minimize disruptions.
- Limit stimulants after 2p.m. Caffeine, nicotine, and even high‑sugar snacks keep the nervous system on edge, worsening both insomnia and pain perception.
- Try a short CBT‑I protocol. Many online platforms offer a 4‑week self‑guided program focusing on stimulus control, sleep restriction, and cognitive restructuring.
- Incorporate gentle movement. A 20‑minute walk, yoga, or tai chi in the late afternoon boosts endorphins, eases muscle tension, and lowers inflammatory cytokines.
- Use a timed melatonin supplement. Take 1mg 30‑60 minutes before bedtime on nights where you struggle to fall asleep.
- Practice mindfulness or deep‑breathing. A 10‑minute body‑scan meditation before bed can quiet racing thoughts and lower cortisol.
- Review pain medication timing. If you take NSAIDs, aim for the morning or early afternoon to avoid nighttime stomach upset that could wake you.

When to Seek Professional Help
If you’ve tried the above steps for four weeks and still wake up feeling exhausted or in constant pain, it’s time to consult a healthcare provider. Look for a specialist who understands the sleep‑pain nexus-often a sleep medicine physician, pain management specialist, or a multidisciplinary clinic.
Key red flags include:
- Sudden onset of severe pain or numbness
- Daytime sleepiness that impacts work or safety (e.g., driving)
- Depression or anxiety that feels unmanageable
- Use of sleep‑affecting substances (opioids, benzodiazepines) without a prescription
Early intervention can prevent the chronic escalation of both conditions.
Quick Checklist: Managing Insomnia‑Pain Cycle
- Maintain a regular sleep‑wake schedule
- Keep the bedroom environment cool, dark, and quiet
- Avoid caffeine & heavy meals after 2p.m.
- Start a CBT‑I or mindfulness routine
- Engage in low‑impact exercise at least three times a week
- Consider timed melatonin (1mg) for sleep onset
- Schedule pain medication earlier in the day
- Consult a professional if symptoms persist >4 weeks
Frequently Asked Questions
Can insomnia cause new chronic pain, or does it only worsen existing pain?
Both. Sleep loss can trigger inflammatory pathways that lead to musculoskeletal soreness, which may evolve into chronic pain if the pattern continues. For people already dealing with pain, insomnia magnifies the perception of that pain, making it feel more severe and harder to manage.
Is it safe to use over‑the‑counter pain relievers at night?
Occasional use is generally safe, but taking NSAIDs right before bedtime can cause stomach irritation and disturb sleep. If you need nighttime pain relief, acetaminophen is often gentler on the stomach, but you should still follow dosage guidelines and discuss chronic use with a doctor.
How long does CBT‑I take to show results?
Most people notice improvements after 4‑6 weeks of consistent practice. The biggest gains usually appear in sleep latency (how fast you fall asleep) and reduced nighttime awakenings.
Do melatonin supplements interfere with pain medication?
Melatonin is generally safe with most analgesics. However, it can increase drowsiness when combined with opioids or sedatives, so start with a low dose and monitor how you feel.
What lifestyle changes have the biggest impact on both sleep and pain?
Regular low‑impact exercise, consistent sleep timing, and stress‑reduction techniques (mindfulness, breathing exercises) are the top three. Together they lower inflammation, balance cortisol, and improve the body’s natural pain‑modulating systems.

9 Responses
Man, that sleep‑pain loop is wild-think of your nervous system as a DJ that just won’t stop cranking the bass when you’re trying to chill.
One night of shredded sleep spikes inflammatory chemicals, and the next morning your muscles feel like they’ve been run over by a truck.
It’s not just in your head; cytokines actually turn up the volume on pain receptors.
That’s why a good night’s rest can feel like a miracle for achy joints.
So if you’re stuck in that vicious cycle, hacking the sleep side is a legit first move.
When the night stretches into a quiet abyss, the mind begins to wander through corridors of regret and unspoken hurts.
In those dim corridors, the body whispers its own grievances, amplifying every throb as though the universe itself were conspiring against comfort.
This is not merely a poetic metaphor; scientific studies reveal that prolonged wakefulness inflames the brain’s microglia, turning them into overzealous sentinels of pain.
As the days accumulate, the feedback loop tightens, and the once‑subtle ache becomes a constant companion, a shadow that never quite lifts.
The philosophical implication is profound: our suffering is both a physiological cascade and an existential narrative we unintentionally author each night.
Yet, within this narrative lies a choice, a silent rebellion against the tyranny of insomnia that can reshape the very pathways of nociception.
By embracing regularity-setting a sanctified hour for the closing of the eyes-we signal to our endocrine system that it may lower cortisol and let serotonin flow.
The simple act of dimming lights an hour before bed becomes a ritual, a pact with the self to honor the body's need for deep, restorative phases.
Mindfulness, too, serves as a lantern, illuminating the dark thoughts that fuel both anxiety and muscular tension.
When you practice a ten‑minute body scan, you invite the parasympathetic nervous system to withdraw its grip, allowing muscles to relax and inflammatory markers to recede.
Moreover, gentle movement in the afternoon-whether a stroll through a park or a low‑impact yoga sequence-dispatches endorphins that act as natural analgesics.
These endorphins not only dull pain but also improve sleep quality by stabilizing the internal clock, illustrating the beautiful reciprocity between activity and rest.
And let us not forget the modest power of a timed melatonin dose, a hormone that gently nudges the circadian orchestra back into harmony without the harshness of pharmaceutical sedatives.
Ultimately, the dance between sleep and pain is a choreography we can learn, a rhythm that, once mastered, lets us step out of the night’s oppressive fog.
So remember, each night is an opportunity to rewrite the script, to replace the cacophony of suffering with a softer, more compassionate lullaby for the body and mind.
Hey folks, if you’re feeling trapped in that sleep‑pain loop, start by mapping out a simple bedtime routine.
Consistent lights‑out and a screen‑free half hour can do wonders for resetting your internal clock.
Pair that with a short walk after dinner and you’ll notice your muscles relax faster.
We must confront the ethical dimension of neglecting our own rest, for to deprive the body of sleep is to commit a quiet injustice against ourselves.
The pain that follows is not just a symptom but a moral warning that we have broken the covenant of self‑care.
Choosing a serene sleeping environment, free from clutter and needless noise, is a righteous act of self‑respect.
When we honor the night, we honor the day, and the cycle of suffering begins to loosen its grip.
Good point about consistency; the body really does thrive on predictable cues.
Sounds solid.
Yo, i cant even with how my back goes full on drama mode when i pull an all nighter!!!
It feels like a fireworks show inside my spine, bang bang, pain everywhere.
Honestly, i tried those melatonin pills but the night still feels like a horror flick.
Maybe i need to stop scrolling reddit till 2am, that stuff is pure chaos for my sleep.
Also, i read that a simple 20‑min walk can actually calm the nerves, so i might give that a shot.
Bottom line: if you dont fix the sleep, the pain will keep writing its own tragic comedy.
Totally get that frustration, but you’ve already taken a big step by looking into the science.
Stick with a CBT‑I program for a few weeks; the results often surprise you.
Combine that with a regular evening walk and you’ll likely see both sleep quality and pain levels improve.
Keep at it, and remember progress can be subtle but steady.
Listen, the complacent chatter about “just try a little more sleep” is a pathetic oversimplification that ignores the brutal reality of chronic pain sufferers.
We need to demand better access to multidisciplinary clinics that treat the sleep‑pain nexus holistically, not just toss a melatonin bottle on the counter and call it a day.
Every minute you waste scrolling through random tips is a minute you could be using to schedule that specialist appointment.
Don’t let the healthcare system’s inertia make you feel guilty for seeking aggressive, evidence‑based interventions.
Push for integrated care plans that include physiotherapy, CBT‑I, and proper medication timing-no more half‑measures.
The fight isn’t just personal; it’s a collective stand against a system that normalizes suffering.
Wake up, take action, and break the cycle once and for all.