Angioedema Symptom Checker
This tool helps assess symptoms related to angioedema. It is not a medical diagnosis. If you have severe symptoms, seek emergency care immediately.
Symptom Assessment
Assessment Results
Ever wondered why a simple pollen sneeze can suddenly swell your lips or throat? That unexpected puffiness is often angioedema, and more often than you think it’s sparked by an allergic reaction. Understanding the link helps you spot the warning signs early and get the right care before things get serious.
What Is Angioedema?
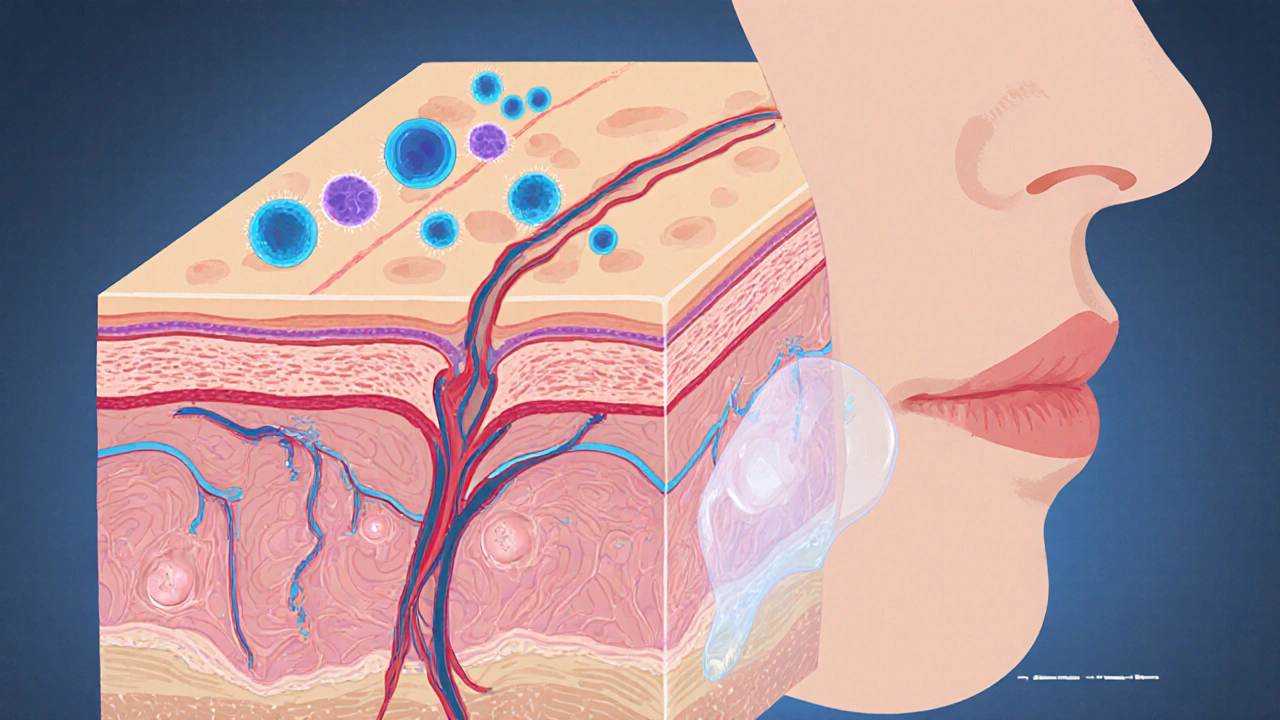
Angioedema is a rapid swelling of the deeper layers of the skin and mucous membranes, usually around the eyes, lips, tongue, or airway. It differs from ordinary hives because the swelling occurs beneath the surface, making it feel like a firm, sometimes painful lump.
How Allergies Lead to Angioedema
Allergic reactions kick off when your immune system mistakenly spots a harmless substance-like pollen, peanuts, or a medication-as a threat. The culprit behind the swelling is a cascade of chemicals released by Mast cells (immune cells packed with granules containing histamine, tryptase, and other mediators) and basophils (a type of white blood cell that also releases histamine during allergic responses).
When an allergen binds to IgE (an antibody type that flags allergens for mast cells and basophils), the cells erupt, dumping histamine into surrounding tissue. Histamine widens blood vessels, allowing fluid to leak into deeper skin layers-hence the characteristic swelling of angioedema.
For many people, this swelling is mild and resolves on its own. But when the airway is involved, the stakes rise dramatically.
Types of Angioedema Linked to Allergies
Not all angioedema stems from the same cause. Below is a quick snapshot of the three most common forms you might encounter.
| Feature | Allergic (IgE‑mediated) | Hereditary (C1‑INH deficiency) | ACE‑Inhibitor‑induced |
|---|---|---|---|
| Typical trigger | Food, insect stings, pollen | Genetic mutation, stress, trauma | ACE‑inhibitor meds (e.g., lisinopril) |
| Onset after exposure | Minutes to hours | Hours to days | Hours to days |
| Primary mediator | Histamine, tryptase | Bradykinin | Bradykinin |
| Response to antihistamines | Usually effective | Limited | Limited |
| Family history | Rare | Common | None |
Allergic angioedema is the form most tied to everyday triggers. Recognising whether histamine or bradykinin is at play guides the right treatment.
Spotting Symptoms Early
- Swelling of lips, eyelids, or tongue that feels “tight” rather than itchy.
- Rapid onset-often within 30 minutes of allergen contact.
- Difficulty speaking, swallowing, or breathing, especially if the throat feels “closed”.
- Accompanying hives (urticaria) suggest an IgE‑mediated process.
- Absence of itching but presence of deep, firm lumps points to non‑histamine (bradykinin) types.
If you notice any throat swelling or trouble breathing, treat it as an emergency. Call emergency services and consider self‑injectable epinephrine if prescribed.
How Doctors Diagnose the Cause
Clinicians start with a detailed history-what you ate, medications you take, and family medical background. Lab tests then narrow the culprit.
- Serum IgE level: Elevated in allergy‑related cases.
- Complement C4 and C1‑esterase inhibitor (C1‑INH) activity: Low levels point to hereditary or acquired angioedema.
- Tryptase: Peaks 1-2hours after an allergic episode, confirming mast‑cell activation.
- Skin prick test or specific IgE blood test: Identifies the exact allergen.
These results help doctors decide whether antihistamines will work or if you need bradykinin‑targeted therapy.
Treatment Options for Allergy‑Related Angioedema
When histamine drives the swelling, the following steps are standard:
- Epinephrine auto‑injector: 0.3mg intramuscular dose for severe throat swelling; it narrows blood vessels and relaxes airway muscles.
- Second‑generation antihistamines: Cetirizine or loratadine, taken every 24hours, block histamine receptors and reduce swelling.
- Corticosteroids: Short courses of prednisone (e.g., 40mg daily for 3‑5days) curb inflammation, especially if symptoms linger.
- Leukotriene receptor antagonists: Montelukast can be added for people who don’t fully respond to antihistamines.
For bradykinin‑mediated cases (hereditary or ACE‑inhibitor), antihistamines and steroids often fall short. Targeted therapies include:
- C1‑INH concentrate: Replaces the missing inhibitor in hereditary angioedema.
- Bradykinin B2‑receptor antagonist: Icatibant, a self‑administered injection that blocks the swelling pathway.
- Fresh‑frozen plasma: In emergency settings when specific drugs aren’t available.
Regardless of the type, early intervention dramatically cuts the risk of airway obstruction.

Managing Triggers and Preventing Recurrence
Prevention works best when you know your personal triggers.
- Allergy testing: Pinpoint foods, insect venoms, or latex that set off reactions.
- Medication review: If you’re on an ACE inhibitor, discuss switching to an ARB with your doctor.
- Carry an epinephrine auto‑injector: Keep it accessible at home, work, and in your bag.
- Wear medical alert jewelry: Simple wording like “Allergic Angioedema - carries epinephrine” saves precious minutes.
- Stress management: For hereditary forms, emotional stress can trigger attacks; techniques such as mindfulness or regular exercise help.
Document each episode-what you ate, meds taken, and symptom timeline. This diary becomes a vital tool for your healthcare team.
Key Takeaways
- Allergy‑related angioedema is a histamine‑driven swelling that can affect lips, eyes, tongue, and airway.
- Fast‑acting epinephrine, antihistamines, and steroids are the frontline treatments for IgE‑mediated attacks.
- Distinguish allergic from bradykinin‑mediated forms; the latter needs C1‑INH or icatibant, not antihistamines.
- Identifying triggers through testing and medication review prevents future episodes.
- Carry emergency medication and wear medical ID - a small step that can save a life.
Frequently Asked Questions
Can a mild allergic rash turn into angioedema?
Yes. In many people, the same allergen that causes itchy hives can also trigger deeper swelling. If you notice any puffiness around the eyes or lips after a rash, treat it as a potential angioedema and watch for airway symptoms.
Why don’t antihistamines help with every angioedema case?
Antihistamines block histamine, the main driver of IgE‑mediated angioedema. However, hereditary and ACE‑inhibitor angioedema are driven by bradykinin, a different molecule. Those cases require bradykinin‑targeted drugs rather than antihistamines.
Is it safe to use an epinephrine auto‑injector if I’m not sure it’s a severe reaction?
Epinephrine is the only medication proven to reverse life‑threatening airway swelling quickly. If you have any doubt about throat involvement, it’s better to use the auto‑injector and seek emergency care.
Can stress alone trigger an angioedema attack?
Stress is a known trigger for hereditary angioedema and can amplify allergic reactions. Managing stress through relaxation techniques can lower the frequency of attacks.
Do children experience allergy‑related angioedema the same way adults do?
Children can develop angioedema, often after food allergies such as nuts or shellfish. Their symptoms may appear more abruptly, and because airway size is smaller, prompt treatment is even more critical.
Understanding how allergy and angioedema intersect gives you the power to act fast, avoid dangerous swelling, and keep your day‑to‑day life running smoothly.

17 Responses
Allergy‑related angioedema is a classic example of how the immune system can overreact to harmless substances. The article correctly highlights the role of mast cells and IgE in the histamine release cascade. It also delineates the distinction between histamine‑mediated and bradykinin‑mediated swelling, which is essential for appropriate therapy. One point worth emphasizing is that not all patients will present with urticaria; deep tissue swelling may occur without itching. Prompt administration of epinephrine remains the cornerstone for life‑threatening airway involvement. For milder cases, a second‑generation antihistamine can be started early to mitigate progression. In cases where antihistamines fail, clinicians should consider a bradykinin blocker or C1‑INH concentrate, especially if the history suggests hereditary angioedema. Overall, the piece serves as a solid reference for both patients and providers.
Hey folks, just a quick heads up – if you ever get that weird tight feeling in your throat, don’t wait, use that epi pen. It’s better safe than sorry, even if you think it’s just a sneeze.
While the article is generally accurate, there are a few linguistic slip‑ups that need correcting. "IgE‑mediated" should be hyphenated throughout, and "bradykinin‑mediated" requires a hyphen as well. Also, the phrase "rapid swelling of the deeper layers" could be refined to "rapid swelling of the deeper dermal layers" for precision. These minor edits will enhance the article’s professional tone.
Ugh, the swelling drama is just too much!
First, let me say thank you for such a comprehensive overview – it’s rare to find a piece that balances basic science with practical tips so well. The step‑by‑step breakdown of the immunologic cascade, from allergen exposure to mast cell degranulation, provides a clear mental model for anyone trying to understand why their lips suddenly puff up. Second, the article does a great job differentiating histamine‑driven from bradykinin‑driven pathways; that distinction is crucial because it directly informs treatment choices. Third, the inclusion of real‑world recommendations – such as carrying an epinephrine auto‑injector and wearing medical alert jewelry – translates knowledge into actionable safety measures. Fourth, the tables summarizing triggers, onset times, and therapeutic responses are a handy reference for clinicians and patients alike. Fifth, I appreciate the emphasis on diagnostic work‑ups like serum tryptase and C1‑INH activity, which can prevent misdiagnosis. Sixth, the discussion about ACE‑inhibitor–induced angioedema reminds prescribers to consider medication reviews in unexplained cases. Seventh, the article rightly warns that airway involvement supersedes all other concerns, urging immediate emergency care. Eighth, the lifestyle tips – stress management, allergen avoidance, and thorough episode documentation – empower patients to take control of their condition. Ninth, the FAQ section anticipates common worries and dispels myths, such as the misconception that antihistamines work for every type of swelling. Tenth, the mention of newer bradykinin‑targeted therapies, like icatibant, reflects up‑to‑date clinical practice. Eleventh, the clear language avoids overly technical jargon, making the content accessible without sacrificing accuracy. Twelfth, the visual cues (like bold headings) guide readers through a potentially overwhelming topic. Thirteenth, the reminder to seek professional evaluation before self‑medicating underscores patient safety. Fourteenth, the piece balances optimism – most attacks are manageable – with sobering realism about the potential for rapid deterioration. Finally, this article serves as an excellent educational tool for both patients navigating daily triggers and clinicians reinforcing best practices.
Excellent article!!! However, note the following: – The term "IgE‑mediated" should always be hyphenated; – "C1‑INH" is often written with a hyphen; – Consistency in bullet‑point formatting improves readability. Keep up the good work! 😊
Honestly, this reads like a textbook summary. The tone is too sterile for a subreddit where people want quick, digestible advice. Trim the fluff and give us the bullet points of what to do when you feel that tongue swelling – that’s what matters.
Wow, such a deep dive! 😲 I’m just here wondering if the article mentioned that some people experience swelling after a night out of drinks 🍻 – definitely worth adding a note about alcohol as a potential co‑trigger!
From a pathophysiological perspective, the cascade can be modeled as a series of amplification loops: allergen‑IgE binding → FcεRI cross‑linking → phospholipase C activation → intracellular calcium influx → degranulation. This leads to a rapid increase in vascular permeability, quantified as an elevated Starling coefficient. Clinicians should therefore monitor hemodynamic parameters in severe cases.
Ths aritlcle iz awsome but i think it shuld mention that some ppl get swulling after they eat chipz. Also, the medecine list could use a bit more drama, lol.
While the content is solid, note that "epinephrine" should be capitalized as a proper noun when referring to the drug brand name, e.g., "Epinephrine auto‑injector." Also, "C1‑INH concentrate" needs a hyphen for consistency.
👍 Got it! Thanks for the grammar tips – will keep an eye on hyphens. Also, adding a smiley really brightens the read! 😊
Oh great, another post telling us to call 911. As if we didn’t already know that…
Helpful summary, especially the part about documenting triggers. Keeps the doctor on the same page and can reduce repeat emergencies.
Well, if you’re going to binge‑read a medical article, at least sprinkle some emojis for flavor 🌶️. Also, did you know “bradykinin” sounds like a fantasy character? Could be a cool boss in a video game.
Thiss articall gutss tho seim bldf knwtht. Alzerteds be frk.
Interesting read. I’ll keep it in mind.