When your heart stops getting the blood it needs, time becomes the enemy. Every minute without treatment kills about 1.5 million heart cells. That’s not a metaphor-it’s science. And the difference between life and death often comes down to whether someone recognizes the signs early enough to call 911.
What a Heart Attack Really Feels Like
Most people picture a heart attack as sudden, crushing chest pain. But that’s only part of the story. The real warning signs are messier, quieter, and often mistaken for something else. The American Heart Association describes it as uncomfortable pressure, squeezing, fullness, or pain in the center of the chest that lasts more than a few minutes-or comes and goes. It doesn’t have to be sharp. It can feel like an elephant sitting on your chest, or just a deep ache that won’t go away. But here’s what most don’t realize: chest pain isn’t always the main symptom. About 65% of people feel discomfort elsewhere-arms, back, neck, jaw, or even the stomach. One woman in Norwich thought she had food poisoning because she was vomiting and had a dull ache under her ribs. It was a heart attack. Another man felt his left arm go numb while gardening and assumed it was a pinched nerve. He didn’t call for help until he collapsed. Shortness of breath is another major red flag. It can happen with or without chest pain. In fact, 40% of heart attack patients report trouble breathing as their first symptom. Some describe it like trying to breathe through a straw. Others feel like they’ve run a marathon when they haven’t moved from the couch. Then there are the less obvious signs: breaking out in a cold sweat for no reason, nausea, dizziness, or an unusual wave of fatigue. Women are especially likely to feel extreme tiredness-nearly half report it as a key warning. One 68-year-old woman said she spent three days feeling "just drained," like her body had been drained of energy. She didn’t think it was serious until she woke up in the hospital.Gender Differences: Why Women’s Symptoms Are Overlooked
Men and women don’t have the same heart attack experience. About 90% of men feel chest pain during a heart attack. Only 64% of women do. That gap is deadly. Women are 58% more likely to have shortness of breath as their main symptom. They’re 47% more likely to feel nauseous or throw up. And they’re 37% more likely to have back or jaw pain without any chest discomfort at all. These are the symptoms doctors call "atypical." But they’re not rare-they’re common. The result? Women are 50% more likely to be misdiagnosed in emergency rooms. One study found that women under 55 are twice as likely as men to be sent home with a diagnosis of anxiety or indigestion-when it’s actually a heart attack. A 42-year-old woman in London was told her jaw pain was TMJ. It took 48 hours and a second ER visit before her heart attack was caught. Even the way women describe their pain is different. Instead of saying "sharp pain," they say "pressure," "tightness," or "heaviness." That language gets misinterpreted. And because heart disease has long been seen as a "man’s disease," many women-and even some doctors-don’t connect the dots.Age Matters Too
Heart attacks aren’t just for older people. The number of heart attacks in adults aged 25 to 44 has been rising by 2% every year since 2000. Younger people often ignore symptoms because they think they’re too healthy to have one. For those over 75, the risk of a "silent" heart attack increases. About 30% of heart attacks in this group happen without chest pain at all. People might just feel unusually tired, dizzy, or have an upset stomach. They might not even realize something’s wrong until it’s too late. Silent heart attacks are especially dangerous because they don’t trigger the alarm bells. People don’t call 911. They wait. And by the time they do, damage is already done.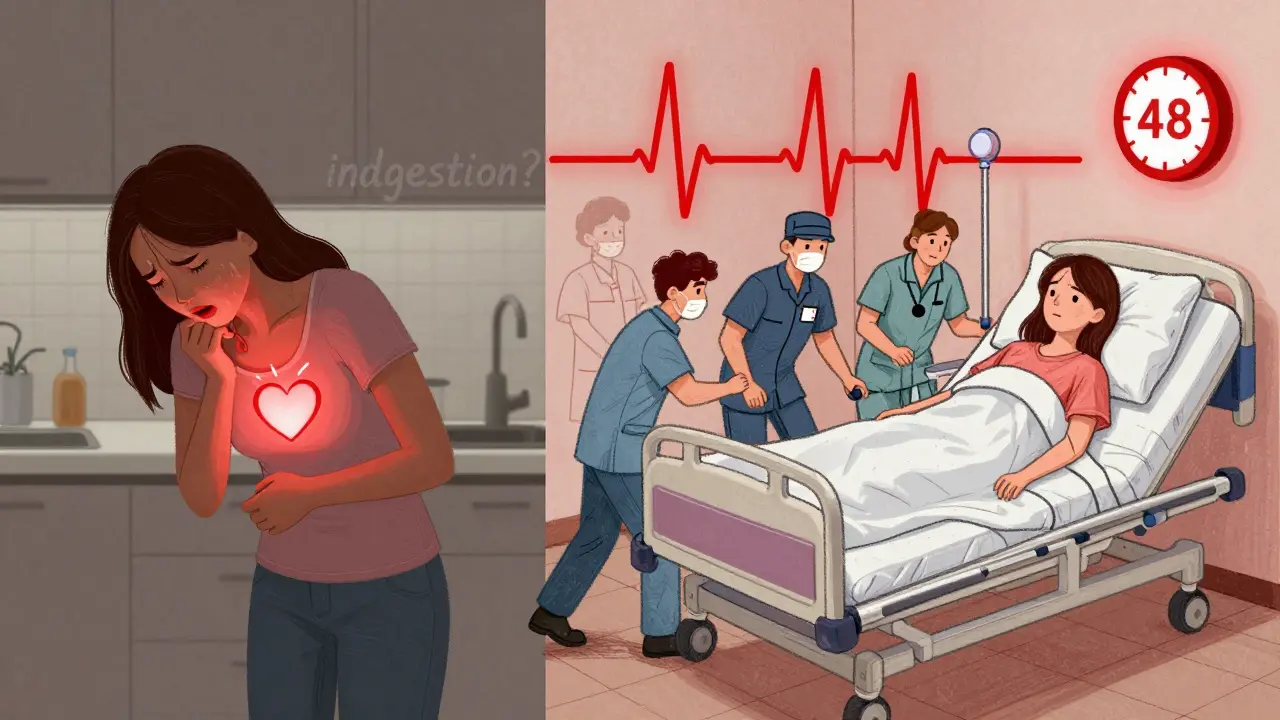
What to Do When You Suspect a Heart Attack
If you or someone else has any of these symptoms-chest pressure, shortness of breath, nausea, cold sweat, jaw or arm pain, unexplained fatigue-don’t wait. Don’t hope it goes away. Don’t text a friend first. Call emergency services immediately. Why? Because ambulances can start treatment on the way to the hospital. They can give oxygen, aspirin, and monitor heart rhythms before you even arrive. People who call 911 get to the hospital 25% faster than those who drive themselves. While you wait for help, chew one 300mg aspirin if you’re not allergic and your doctor hasn’t told you to avoid it. Aspirin helps thin the blood and can reduce damage to the heart. Don’t take it if you’re unsure-just call 911. And if you’re with someone who collapses, starts gasping, or becomes unresponsive, start CPR right away. Even if you’ve never done it before, pushing hard and fast on the center of the chest can keep blood flowing until help arrives. Communities with CPR training have 28% higher survival rates for out-of-hospital cardiac arrests.Why People Wait Too Long
The average person waits three hours before calling 911 after symptoms start. That’s three hours too long. Why? Denial is the biggest reason. People think, "It’s probably just indigestion." Or, "I’m not old enough to have a heart attack." Or, "What if I’m wrong? Won’t I look foolish?" A 2023 survey found that 33% of heart attack victims waited more than two hours because they were afraid of embarrassing themselves. One man in Birmingham waited six hours because he didn’t want to "bother" his daughter. He ended up needing a stent and a week in the hospital. Another reason? Uncertainty. A HealthUnlocked survey of 1,200 survivors showed that 52% delayed help because they weren’t sure if their symptoms were serious. Women took longer on average-2.7 hours compared to 1.9 for men. But here’s the truth: it’s better to be wrong and get checked than to be right and die.What’s Changing-And What’s Working
Technology is helping. The FDA approved the first AI-powered heart attack prediction tool in March 2023. It can spot warning signs on an EKG 30 minutes before symptoms appear, with 92.7% accuracy. More people are using smartwatches that detect irregular heartbeats-a known risk factor. Public awareness campaigns are making a difference too. The American Heart Association’s "Go Red for Women" program has reached 85% of U.S. women. In the UK, the British Heart Foundation has trained over 2 million people in CPR since 2020. But the biggest change comes from education. People who’ve taken a 30-minute online course on heart attack symptoms reduce their delay time by nearly 50 minutes. That’s enough to save heart muscle-and lives.What You Can Do Today
You don’t need to be a doctor to save a life. Here’s what to do:- Know the symptoms-not just chest pain, but also shortness of breath, nausea, jaw pain, cold sweat, and extreme fatigue.
- Teach your family, especially women and older adults, that heart attacks don’t always look like the movies.
- Keep aspirin in your medicine cabinet if you’re not allergic.
- Learn basic CPR. It takes less than 10 minutes to learn online.
- If you feel something’s wrong-call 999. Don’t wait. Don’t second-guess.

8 Responses
Let’s be brutally honest-this post is a masterclass in oversimplification. The notion that ‘chewing aspirin’ is some universal panacea? That’s medical malpractice waiting to happen. Aspirin isn’t a magic bullet; it’s an anticoagulant with contraindications-GI bleeds, Reye’s syndrome, NSAID hypersensitivity-and you’re just telling people to pop one like a candy?!
And don’t even get me started on the AI prediction tool. FDA-approved? Sure. But validated on what dataset? Whitewashed cohorts? Where’s the peer-reviewed publication? This reads like a marketing pamphlet disguised as public health guidance.
Also-‘silent heart attacks’? Please. That’s not a medical term. It’s a euphemism for ‘undiagnosed myocardial infarction.’ We don’t need euphemisms; we need precision. And stop romanticizing CPR like it’s a TikTok challenge. Proper chest compressions require training. Not ‘watch a 10-minute video’ nonsense.
And who wrote this? Someone who’s never seen a real EKG? The difference between ischemia and pericarditis isn’t something you learn from a BuzzFeed list. This post is dangerously reductive.
Also: why no mention of troponin levels? Or the fact that 40% of MI cases present with normal EKGs? You’re not educating-you’re performative altruism with bullet points.
And yet… I’m still glad someone wrote it. Because ignorance is deadlier than misinformation. But please. Next time, cite your sources. Or at least don’t pretend this is science.
This is important stuff. I’m a nurse, and I’ve seen too many people wait too long-especially women. One lady came in thinking she had the flu. Turns out, her heart was 70% blocked. She didn’t even have chest pain.
Just remember: if something feels off, trust it. You don’t need to be an expert to save a life. Call 911. No shame. No hesitation.
And yes-CPR works. Even if you’re not perfect. Just keep pushing.
Oh wow. So now we’re supposed to believe that ‘jaw pain = heart attack’? Next you’ll tell me my hangover is a silent MI.
And let’s not forget the ‘300mg aspirin’ advice. Because clearly, the CDC doesn’t have a problem with people self-prescribing blood thinners based on a Reddit post.
Also, ‘women are 58% more likely to have shortness of breath’? Source? Is that from the same study that said ‘men are 100% more likely to be idiots’?
Look-I get it. You want people to act. But this isn’t education. It’s fear-mongering with emojis.
They don’t want you to know the truth. 🤫
Heart attacks aren’t natural. They’re engineered. The pharmaceutical companies need you to think it’s ‘lifestyle’-so you’ll keep buying statins, aspirin, and EKG machines. Meanwhile, the real cause? 5G radiation. And the fact that your smartwatch is silently monitoring your heartbeat… for who? Who’s collecting that data?
And why is the FDA approving ‘AI tools’ right after the 2020 election? Coincidence? I think not.
Also-CPR? They train you to push on the chest… but what if that’s where the microchip is? 😈
Call 911? Nah. Call your local prepper group. Bring a tourniquet. And a Faraday cage.
They want you scared. So you’ll obey. Don’t be a sheep.
Thank you for sharing this vital information with such clarity and compassion.
I have spent over two decades working in emergency care, and I can confirm: early recognition saves lives. The hesitation to call for help is often rooted in fear-fear of being wrong, fear of burdening others, fear of the unknown.
But let me say this plainly: you are never a burden for choosing life. Your instinct to seek help is not weakness-it is courage.
And to those who say, ‘I’m too young’-you are not invincible. Heart disease does not discriminate by age. It discriminates by silence.
Please. If you feel something is wrong-act. Even if it’s just a whisper.
Bro, I thought I had food poisoning last year. Just nausea, weird sweating, left arm numb. Went to urgent care. They said ‘virus.’
Turned out it was a mini heart attack. No chest pain. Just… gone.
Now I keep aspirin in my wallet. And I tell everyone I know. Seriously. Don’t wait.
While the intent of this article is commendable, its rhetorical structure betrays a fundamental misunderstanding of medical communication. The conflation of statistical correlation with deterministic causality-particularly in the gender-based symptom analysis-risks reinforcing diagnostic bias rather than mitigating it.
Moreover, the uncritical endorsement of AI-driven EKG interpretation, without acknowledging its dependence on training data that underrepresents non-Caucasian populations, is ethically indefensible.
Public health messaging must be precise, evidence-based, and cognizant of systemic inequities-not performative.
Thank you for writing this. I shared it with my mom, my sister, and my 28-year-old nephew. 💙
My aunt died because she thought her fatigue was ‘just aging.’
Let’s change that. For everyone.