Antihistamine Drowsiness Duration Calculator
How Long Will You Be Drowsy?
Estimate the duration of drowsiness effects from first-generation antihistamines based on your specific situation. This tool helps you understand when it's safe to drive or operate machinery.
Estimated Drowsiness Duration
Important Safety Note
First-generation antihistamines are everywhere - in your medicine cabinet, at the pharmacy checkout, even in some sleep aids labeled as "natural." But behind their low price and quick relief lies a hidden cost: intense drowsiness and a range of troubling side effects that can linger for hours, sometimes days. These aren’t just mild inconveniences. For many people, especially older adults, they’re a silent threat to cognitive health, safety, and daily function.
What Exactly Are First-Generation Antihistamines?
These are the original antihistamines developed in the 1940s and 1950s, like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), promethazine (Phenergan), and hydroxyzine (Atarax). They work by blocking histamine, the chemical your body releases during an allergic reaction. But unlike newer versions, they don’t stop there. Their small, oily molecular structure lets them slip easily through the blood-brain barrier. Once inside the brain, they bind to H1 receptors - but also to muscarinic receptors, which control things like saliva, bladder function, and memory.
This dual action is why they’re effective for allergies, motion sickness, and even insomnia. But it’s also why they cause dry mouth, blurred vision, trouble peeing, confusion, and that heavy, groggy feeling you can’t shake. Studies show brain concentrations of diphenhydramine can hit 15-25 ng/mL within two hours - enough to impair reaction time as much as being legally drunk. Second-generation antihistamines like cetirizine or loratadine? Their brain levels stay under 1 ng/mL. The difference isn’t subtle. It’s life-altering.
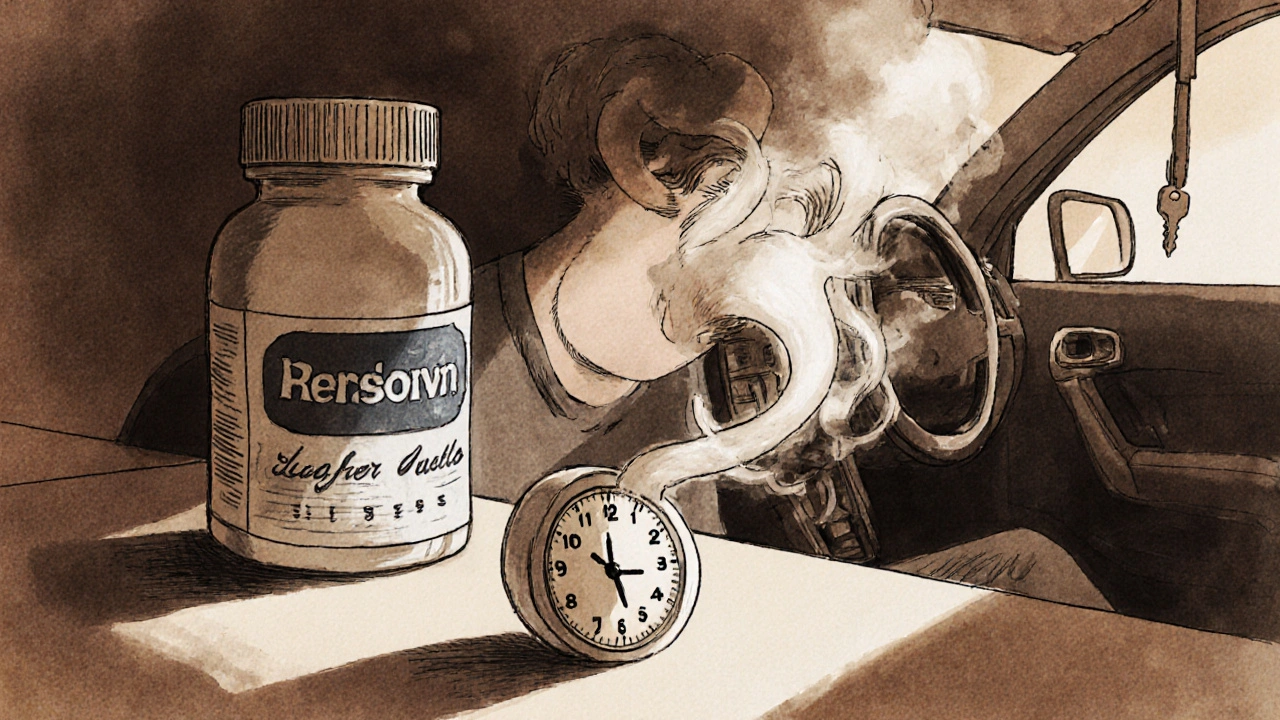
The Drowsiness Isn’t Just "Feeling Tired" - It’s a Safety Risk
When people say they feel "a little sleepy" after taking Benadryl, they’re underestimating what’s happening. This isn’t a gentle nod-off. It’s deep sedation. Driving simulators show first-generation antihistamines reduce reaction times by 30-50%. One study found impairment lasted up to 18 hours after a single dose. That means taking it at 8 p.m. for allergies doesn’t just help you sleep - it leaves you impaired the next morning, even if you feel "fine."
Real-world data backs this up. In 2021, 35% of emergency department visits for drowsy driving involved first-generation antihistamines, according to NHTSA. People don’t realize they’re impaired until it’s too late. A Reddit user wrote: "Took Benadryl at 8 PM for hives and woke up at 2 PM the next day feeling like I’d been hit by a truck - not worth it for mild allergies." That’s not an outlier. On Drugs.com, 38% of 3,782 users reported "extreme sleepiness" after diphenhydramine.
And it’s not just driving. Operating machinery, caring for children, or even walking down stairs becomes risky. The fog isn’t temporary. It’s pharmacological. Your brain is literally being slowed down by the drug.
Anticholinergic Effects: More Than Just Dry Mouth
Anticholinergic side effects aren’t just annoying - they’re dangerous, especially with long-term use. These drugs block acetylcholine, a key neurotransmitter for memory, attention, and muscle control. The result? Dry mouth, constipation, urinary retention, blurred vision, and cognitive fog.
For older adults, this is catastrophic. The American Geriatrics Society lists first-generation antihistamines as "potentially inappropriate" for people over 65. Why? Chronic use increases dementia risk by 54%. That’s not a small uptick. That’s a major public health concern. A 2022 survey of 1,204 older adults found 42% experienced morning confusion lasting 3-4 hours after nightly use - and many didn’t connect it to the pill they took.
Even younger people aren’t immune. WebMD forums report 28% of long-term users developed urinary issues - difficulty starting or stopping urine flow - consistent with anticholinergic bladder effects. One user described needing artificial saliva products because their mouth felt "like sandpaper." These aren’t rare side effects. They’re predictable, well-documented, and avoidable.

Why Do People Still Use Them?
If they’re this risky, why are they still on shelves? Three reasons: price, availability, and myths.
First, they’re cheap. A bottle of 24 diphenhydramine tablets costs about $5. The same number of loratadine tablets? Around $15. For people without insurance or on tight budgets, the cost difference is hard to ignore.
Second, they’re easy to get. You don’t need a prescription. OTC packaging often downplays the risks. The label might say "may cause drowsiness," but it doesn’t scream "this could impair you for half a day." A 2022 JAMA study found 45% of users underestimated how long the effects would last.
Third, people believe the myth that "it’s just a sleep aid." Many older adults take low-dose diphenhydramine nightly because they’ve been told it’s safe. But sleep isn’t the same as rest. These drugs don’t improve sleep quality - they suppress wakefulness. The next-day grogginess? That’s not a side effect. That’s the drug still working.
When Might They Still Be Okay to Use?
They’re not all bad. There are specific situations where their benefits outweigh the risks - but only if used carefully.
- Motion sickness: First-generation antihistamines like dimenhydrinate (Dramamine) are more effective than newer ones for preventing nausea on boats or planes. Dose 30-60 minutes before travel. Avoid driving afterward.
- Short-term insomnia: If you’re having a single bad night and can’t sleep, a low dose (12.5-25 mg) of diphenhydramine might help. But don’t use it nightly. The brain adapts, and the risk of cognitive decline climbs.
- Acute allergic reactions: For severe hives or swelling, they work fast - within 15-30 minutes. But switch to a second-generation antihistamine once the crisis passes.
Always take them at bedtime. Never mix them with alcohol - it boosts brain penetration by 40-60%. And if you’re over 65, pregnant, or taking other medications (especially antidepressants or painkillers), talk to a pharmacist before using them.

What Should You Use Instead?
For daily allergy relief, second-generation antihistamines are the clear choice: cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra), and desloratadine (Clarinex). They’re non-sedating, last 12-24 hours, and don’t affect your memory or bladder.
For sleep, try melatonin, magnesium, or behavioral changes like reducing screen time before bed. For motion sickness, consider ginger supplements or acupressure bands. For chronic allergies, nasal corticosteroids like fluticasone are more effective and safer long-term.
The bottom line? First-generation antihistamines have a place - but it’s narrow. They’re not for daily use, not for driving, and not for older adults. If you’re using them regularly, ask yourself: Is this helping me - or just masking the problem with a side effect that’s hurting me more?
What’s Changing? The Future of Antihistamines
Regulators are catching up. The UK banned over-the-counter promethazine for minors in 2022. The FDA is considering similar restrictions on diphenhydramine after pediatric ER visits rose 27% from 2018-2022. New labeling guidelines now require stronger warnings about next-day impairment.
Pharmaceutical companies are working on "third-generation" antihistamines designed not to cross the blood-brain barrier at all. Two candidates, EB-029 and DP-118, are in Phase II trials and show 80% less brain penetration while keeping the allergy-fighting power. These could be game-changers - but they’re years away.
In the meantime, the message is clear: don’t reach for Benadryl because it’s cheap or convenient. If you need relief without the fog, there are better options. And if you’ve been using these pills for years, it’s not too late to switch. Your brain will thank you.
Are first-generation antihistamines safe for older adults?
No. The American Geriatrics Society strongly advises against their use in people over 65. These drugs increase the risk of cognitive decline, confusion, falls, and dementia by up to 54% with long-term use. Even low doses taken nightly can cause next-day brain fog that lasts hours. Safer alternatives like nasal sprays or second-generation antihistamines should be used instead.
How long does drowsiness from Benadryl last?
Drowsiness typically starts within 30 minutes and peaks at 1-2 hours after taking it. But impairment can last 6-18 hours, depending on your metabolism. Some people feel groggy the next morning, even if they slept well. Driving or operating machinery during this window is dangerous. Studies show reaction times remain impaired for up to 18 hours after a single dose.
Can first-generation antihistamines cause urinary problems?
Yes. By blocking acetylcholine in the bladder, these drugs can cause urinary retention - difficulty starting urination, weak stream, or feeling like your bladder isn’t empty. This is especially common in older men with enlarged prostates. One study found 28% of long-term users on WebMD forums reported these symptoms. If you’re having trouble peeing after taking diphenhydramine or similar drugs, stop using them and talk to a doctor.
Is it safe to take first-generation antihistamines with alcohol?
No. Alcohol increases how much of the drug enters your brain by 40-60%. This dramatically worsens drowsiness, dizziness, and loss of coordination. The combination can lead to falls, accidents, or even respiratory depression. Never mix these medications with alcohol - even one drink.
What are the best non-drowsy alternatives for allergies?
For daily allergy relief, use second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra), or desloratadine (Clarinex). They’re non-sedating, last 12-24 hours, and don’t impair memory or reaction time. For nasal symptoms, fluticasone (Flonase) or mometasone (Nasonex) nasal sprays are more effective and have no systemic side effects. These are safer long-term options.
What to Do Next
If you’re currently using a first-generation antihistamine daily - for allergies, sleep, or anything else - take a moment to reassess. Ask yourself: Is this helping me, or am I just trading one problem for another? Talk to your pharmacist or doctor. Ask about switching to a non-sedating option. If you’re using it for sleep, consider a sleep hygiene plan instead. If you’re using it for allergies, try a nasal spray. Your brain, your bladder, and your safety are worth more than the $5 savings.
14 Responses
Just had my grandma switch from Benadryl to loratadine last month. She’s been sleeping better, not stumbling in the hallway, and actually remembered my birthday. No more morning fog. It’s not magic-it’s just pharmacology. Why do we accept this level of cognitive erosion as normal?
The blood brain barrier is not a filter it is a gatekeeper and first generation antihistamines are the brute force entry team that kicks it in and then takes a nap on the couch inside the house of the mind
So what you're saying is... we should all be rich and have insurance? Cool. I'll wait for the third-gen magic pill while my allergies rage.
It is not merely a matter of pharmacokinetics but of societal negligence. The commodification of sedation as a therapeutic modality reflects a broader epistemological failure in public health discourse. The normalization of cognitive impairment as an acceptable trade-off for convenience is not benign-it is a form of structural violence.
They're hiding something... these 'second-gen' drugs are just the same but with a new label. Big Pharma wants you to pay more and they control the FDA. I saw a guy on YouTube say the brain fog is actually a chip being activated. Why do you think they don't warn about this? 🤔
If you're still using Benadryl for sleep, you're not just stupid-you're dangerous.
Second-gen? More like second-rate. Benadryl works. Period. You want to feel like a zombie? Fine. I'll take the $5 pill and sleep like a log. You want to pay $15 to feel awake? Go ahead. I'm not your guinea pig.
Think about it-our whole culture is built around masking symptoms instead of fixing causes. We don’t ask why we’re allergic. We just pop a pill. We don’t fix sleep hygiene-we take a sedative. We’re not treating ourselves. We’re outsourcing our biology to a bottle.
I used to take diphenhydramine every night for years. Thought it was harmless. Then I started forgetting where I put my keys. Then I forgot my daughter’s recital. Then I fell down the stairs. Three ER visits later, my neurologist said, 'You’ve been self-administering early-onset dementia.' I stopped. My brain didn’t come back-but it stopped getting worse. This isn’t a warning. It’s a eulogy for your future self.
my mom took this for years and never said anything... now she says she feels "clearer" since switching. i'm glad i read this. 🫂
Thank you for writing this with such clarity and care. As a nurse, I see the fallout every day-older patients confused, falling, unable to concentrate. We need better education, not just better drugs. This should be required reading in every high school health class.
Man, I used to think Benadryl was the cool kid on the block-cheap, fast, got the job done. Then I took it before a road trip and spent 12 hours staring at a gas station sign like it was a hologram. That was the day I realized: some things aren’t worth saving $10 on. Now I use Zyrtec and actually enjoy my weekends.
Why are Americans so weak? In Nigeria, we take whatever works. If a pill makes you sleepy, you sleep. You don’t whine about brain fog. You adapt. Your country is full of people who think a nap is a medical condition. Get stronger.
Wait, so you’re saying I shouldn’t use Benadryl to help my toddler sleep? But it’s the only thing that works! I’ve tried everything else. What am I supposed to do?