For millions of people living with fibromyalgia, pain isn’t just a symptom-it’s the constant background noise of everyday life. Imagine waking up every morning feeling like you’ve been hit by a truck, your muscles aching all over, your mind foggy, and your sleep never quite deep enough. No matter how much you rest, the pain doesn’t go away. And when you go to the doctor, you’re often told it’s "all in your head." That’s the cruel reality for many with fibromyalgia: a real, measurable neurological condition that’s still misunderstood, even by some in the medical community.
What Fibromyalgia Actually Is
Fibromyalgia isn’t arthritis. It’s not muscle strain. It’s not depression. It’s a chronic disorder where the central nervous system amplifies pain signals. The body’s pain processing system gets stuck on high volume. This isn’t just about sore muscles-it’s about how your brain and spinal cord interpret sensations. Even light touch can feel painful. A hug might hurt. A breeze against your skin can feel like sandpaper. The American College of Rheumatology defines it by three key things: widespread pain lasting at least three months, fatigue that doesn’t improve with rest, and cognitive issues-what patients call "fibro fog." You might forget where you put your keys, struggle to find the right word, or lose track of conversations. And sleep? Most people with fibromyalgia don’t reach deep, restorative stages. They wake up tired, even after eight hours. It affects 2 to 8% of people worldwide. About 80% of those diagnosed are women. That doesn’t mean men don’t get it-they do-but they’re often misdiagnosed or told it’s stress. Diagnosis takes years on average-five, according to research. Many patients see five or more doctors before getting the right label.Why Antidepressants Are Used-And Why They’re Not What You Think
When you hear "antidepressant," you might think: "They think I’m depressed." That’s the biggest myth. Antidepressants like duloxetine, amitriptyline, and milnacipran are prescribed not because patients are sad-they’re prescribed because they change how the brain handles pain. These drugs work on neurotransmitters: serotonin and norepinephrine. These chemicals don’t just affect mood-they’re part of the body’s natural pain control system. In fibromyalgia, that system is broken. Antidepressants help restore some of that balance, quieting the overactive pain signals. The FDA has approved three drugs specifically for fibromyalgia: duloxetine (Cymbalta), milnacipran (Savella), and pregabalin (Lyrica). But amitriptyline, an older tricyclic antidepressant, is still widely used-even though it’s not FDA-approved for this use. Why? Because it works. A 2022 review found it reduces pain by about 30% and improves sleep in 6 to 8 weeks. And sleep is huge. When you sleep better, pain feels less intense. But here’s the catch: these drugs don’t work for everyone. Studies show only about half of patients get meaningful pain relief. And side effects? They’re real. Dry mouth, drowsiness, weight gain, nausea, dizziness. Some people feel worse before they feel better. One patient on r/fibromyalgia wrote: "Duloxetine at 60mg gave me panic attacks. I had to quit." That’s not rare. Around 25-30% of people stop taking these meds because of side effects.The Real Hero: Exercise (Yes, Really)
If you’ve ever been told to "just move more" for fibromyalgia, you’ve probably rolled your eyes. How do you move when even walking to the fridge feels impossible? But here’s the truth: exercise is the most effective treatment we have. It’s not about running marathons. It’s about starting small. The American College of Rheumatology recommends beginning with 15 to 20 minutes, two or three times a week. Low-impact activities like walking, swimming, tai chi, or yoga. Tai chi, in particular, has been shown to reduce pain by 20-30% in just 12 weeks. Yoga? One study found a 24% drop in pain intensity after 12 weeks of regular practice. The key is pacing. Go too hard, and you’ll flare up. The rule of thumb? Increase activity by no more than 10% per week. A 5-minute walk today? Next week, try 5.5 minutes. That’s it. Consistency beats intensity every time. Patients who stick with exercise report long-term improvements-better sleep, less pain, more energy. A 2023 survey of over 1,200 patients found 68% said exercise was the most helpful thing they’d done. That’s higher than any medication.
How Medication and Exercise Work Together
Antidepressants aren’t the enemy. But they’re not the whole answer. Think of them as a bridge-not a destination. Many people start with a low dose of amitriptyline (5mg at bedtime) to help with sleep. Within a few weeks, they begin gentle stretching or walking. As their body adjusts, they slowly increase movement. After 6 to 8 weeks, they might add tai chi or water aerobics. The medication helps them get through the initial pain barrier so they can start moving. Movement then builds resilience. The body learns it’s safe to move again. A 2022 Arthritis Foundation survey found that 37% of patients who saw the best results used a combination: low-dose antidepressant (like 20mg duloxetine) plus tai chi three times a week. That’s not a coincidence. The drug helps with the immediate pain and sleep. The exercise rebuilds the nervous system’s tolerance.What Doesn’t Work-and What’s Coming Next
Opioids? They’re not recommended. They don’t help fibromyalgia pain and carry serious risks. Steroids? No benefit. Anti-inflammatories? Usually useless-this isn’t inflammation-driven pain. Cognitive Behavioral Therapy (CBT) is another powerful tool. It doesn’t mean "think positive." It means learning how to manage flare-ups, break the cycle of pain-fear-inactivity, and reframe thoughts like "I can’t do anything" into "I can do a little today." Studies show CBT improves pain and function by 20-30% over 8 to 12 weeks. And the future? Promising. The FDA accepted a new drug called centanafadine in early 2024. Phase 3 trials showed 35% pain reduction with fewer side effects than current options. Researchers are also exploring brain stimulation devices like the Quell device, which sends gentle pulses to nerves to block pain signals. And NIH just allocated $15 million in 2023 to study how fibromyalgia affects brain chemistry-finally treating it like the neurological condition it is.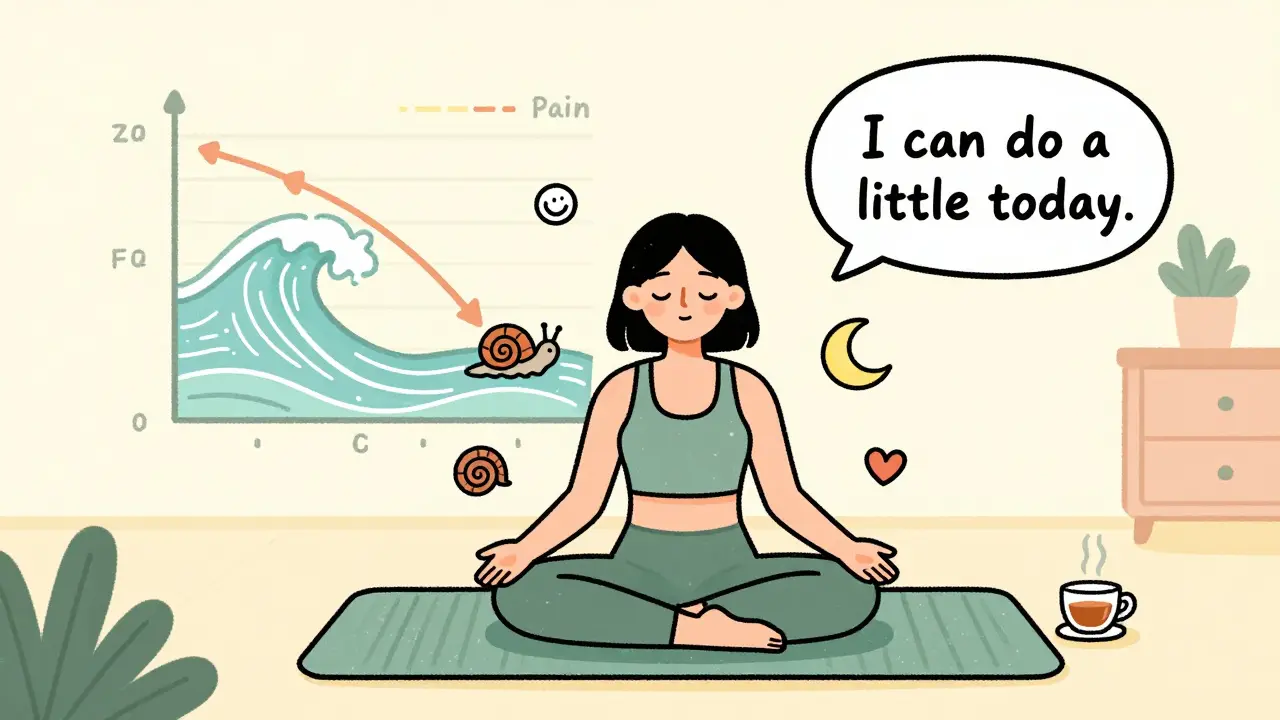
Practical Steps to Start Today
If you’ve been diagnosed-or suspect you have fibromyalgia-here’s what to do next:- Get educated. Use the CDC’s free "Managing Fibromyalgia" online course. Know what you’re dealing with.
- Start moving. Walk for 5 minutes today. Tomorrow, 6. Keep going. Don’t wait for pain to disappear-move through it slowly.
- Track your sleep. Poor sleep makes everything worse. Try a consistent bedtime, no screens an hour before bed, and consider low-dose amitriptyline if sleep is your biggest issue.
- Ask about meds wisely. If your doctor suggests an antidepressant, ask: "What’s the goal?" and "What side effects should I watch for?" Start low. Go slow.
- Find support. Join a group. Online or in person. You’re not alone. And you don’t have to figure this out by yourself.
What to Expect in the First Few Months
The first 4 to 8 weeks are about building a foundation. You’re not fixing this overnight. You’re learning to live with it differently. - Weeks 1-4: Focus on sleep and gentle movement. Medication, if started, begins at the lowest dose. Expect minor side effects. Don’t panic. They often fade.Final Thought: You’re Not Broken
Fibromyalgia isn’t your fault. It’s not weakness. It’s not "just stress." It’s a real, complex condition of the nervous system. And while there’s no cure, there is control. You can build a life where pain doesn’t rule you. The most effective treatment isn’t a pill. It’s a combination: movement, sleep, support, and-when needed-medication that helps you get to the point where movement becomes possible. You don’t need to be cured to live well. You just need to find what works-for you.Are antidepressants addictive for fibromyalgia?
No, antidepressants used for fibromyalgia-like duloxetine, amitriptyline, or milnacipran-are not addictive. They don’t create a high or lead to cravings. But they can cause withdrawal symptoms if stopped suddenly, like dizziness or nausea. That’s why doctors recommend tapering off slowly, not quitting cold turkey. This is not addiction-it’s physical adjustment.
Why do some doctors still prescribe opioids for fibromyalgia?
They shouldn’t. Major guidelines from the CDC, American College of Rheumatology, and FDA all warn against opioids for fibromyalgia. They don’t reduce central pain and carry high risks of dependence, overdose, and worsening pain sensitivity over time. Some doctors may prescribe them out of frustration or lack of training, but it’s not evidence-based care. If you’re being offered opioids, ask for alternatives.
Can fibromyalgia go away on its own?
Fibromyalgia is a chronic condition, meaning it doesn’t usually disappear completely. But symptoms can improve significantly with the right management. Many people reach a point where pain is mild, predictable, and doesn’t interfere with daily life. This isn’t a cure-it’s control. And with better treatments emerging, more people are living well with fibromyalgia than ever before.
Is fibromyalgia the same as chronic fatigue syndrome?
They’re closely related but not the same. Both involve fatigue, pain, and brain fog. But fibromyalgia is defined by widespread pain as the main symptom, while chronic fatigue syndrome (ME/CFS) is defined by extreme, unexplained fatigue that doesn’t improve with rest. Many people have both, and the treatments overlap-especially exercise and sleep management. Experts now believe they may be different expressions of the same underlying nervous system dysfunction.
How long does it take for antidepressants to work for fibromyalgia?
It varies. For sleep, tricyclics like amitriptyline can help in 2 to 4 weeks. For pain relief, SNRIs like duloxetine usually take 4 to 6 weeks. But full benefits often take 8 to 12 weeks. Don’t give up after two weeks. If you’re not seeing improvement by 10 weeks, talk to your doctor about adjusting the dose or trying something else.
What if I can’t afford physical therapy or CBT?
You don’t need expensive programs to start. Free resources exist: YouTube has guided tai chi and yoga videos for beginners. The CDC’s online course is free. Apps like Insight Timer offer free mindfulness sessions. Local libraries often host free support groups. Start with what you can do at home-walking, breathing exercises, journaling. Progress matters more than perfection.
Can stress make fibromyalgia worse?
Yes. Stress-emotional, physical, or environmental-triggers flare-ups by overloading the nervous system. That’s why managing stress is part of treatment. Deep breathing, pacing your day, setting boundaries, and saying no aren’t luxuries-they’re medical tools. One patient described it as "turning down the volume on my body’s alarm system."

11 Responses
Man, I’ve been living with this for 12 years. They told me it was anxiety. Then depression. Then ‘you just need to try harder.’ Turned out my nervous system was just screaming into a void. The amitriptyline didn’t fix me, but it let me breathe long enough to start walking again. Small wins, man. Small wins.
Also, Tai Chi saved my life. Not because it’s magic-because it taught me how to move without fighting myself.
so like… pain is just your brain playing loud music on repeat 🎵🔥 and antidepressants? they’re the volume knob 😌 maybe not perfect but hey at least it’s not opioids 🙏 no cap
I’m from a small town where no one believed me either. But I started walking around the block every day. Just five minutes. Then ten. Now I do yoga on YouTube with my cat on my lap. It’s not glamorous. But it’s mine. And I’m still here. That’s enough.
You’re not broken. You’re just wired differently. And that’s okay.
Exercise is the only evidence-based treatment that consistently outperforms meds. Period. Start with 5 minutes a day. Walk, stretch, swim-doesn’t matter. Consistency beats intensity every time. Track progress. Don’t compare day one to month six. You’re rebuilding your nervous system, not running a marathon.
Medication? Use it as a bridge. Not a crutch.
Okay but let’s be real-how many of these ‘success stories’ are just people who had mild cases to begin with? And why is the only solution always ‘move more’? What if you can’t? What if your body literally screams when you try? This whole post feels like a Pinterest board for people who haven’t actually lived this.
And don’t get me started on ‘low-dose amitriptyline.’ I took 10mg for three months. Woke up like a zombie. Weight gain, dry mouth, brain fog so thick I forgot my own birthday. Then they told me to ‘try harder.’
Yeah. I’ll try harder. Right after I stop being gaslit by wellness culture.
Let’s not romanticize the pharmaceutical-industrial complex. Antidepressants are not ‘pain modulators’-they’re Band-Aids on a ruptured artery. And exercise? A well-trodden trope peddled by people who’ve never spent a week bedridden from a flare-up. The real ‘hero’ here is the pharmaceutical lobby, quietly funding ‘research’ that paints these drugs as miracle cures while ignoring neuroinflammation, mitochondrial dysfunction, and trauma’s role in central sensitization.
And don’t get me started on ‘tai chi’ as a cure-all. If this were truly about science, we’d be funding brain imaging studies, not yoga videos.
Progress? It’s not progress if it’s just distraction dressed up as hope.
I cried when I read this. In Jakarta, my doctor said, ‘You’re too young to have chronic pain.’ I hid my diagnosis for years. Then I found a small group online-just five women, all from different countries. We send each other voice notes when we can’t talk. One said, ‘I walk with my cane like a queen.’ Now I do too.
This isn’t just info. It’s a lifeline. Thank you.
Start small. That’s the mantra. Five minutes. One stretch. One deep breath. That’s victory.
Don’t wait for motivation. Move anyway. Even if it’s slow. Even if it hurts. Your nervous system is learning. It’s not giving up. It’s adapting.
And if you’re on meds? Don’t feel guilty. If it lets you get out of bed, it’s doing its job. You’re not weak-you’re strategic.
You got this. One step. One day. One breath. Repeat.
So we’re telling people their pain is real, but the solution is to move more while on drugs that make them feel like zombies? Interesting. So the body’s alarm system is malfunctioning, but the cure is to install a new alarm system that also makes you sleepy and gain weight?
Reminds me of fixing a leaky roof by putting a bucket under it and calling it ‘innovation.’
Maybe the real question isn’t ‘how do we treat fibromyalgia’-but ‘why did we ignore the nervous system for so long?’
Also, why is ‘exercise’ the only thing that gets called ‘evidence-based’ while everything else is dismissed? Because it’s cheap? Or because it sounds moral?
Look, I’ve tried everything. Medication. Yoga. CBT. Even acupuncture that cost me $300 and did nothing. The only thing that helped? A therapist who didn’t say ‘just move more’ and actually listened. She said, ‘Your body isn’t broken-it’s overwhelmed.’
That changed everything.
Now I do 10 minutes of breathing. I say no to things. I nap without guilt. And I let myself be tired.
It’s not about fixing. It’s about surviving with dignity.
Also, I still hate mornings. But now I hate them on my terms.
Just wanted to say thanks for writing this. I’ve been too scared to tell my doctor I think I have fibro. Now I’m going. And I’m starting with a 5-minute walk tomorrow. No pressure. Just… one step.