Dofetilide Heartburn Safety Checker
Is Your Heartburn Relief Safe with Dofetilide?
This tool helps you understand whether your heartburn medication is safe to take if you're on dofetilide (Tikosyn). The interaction between these drugs can cause deadly heart rhythms. Always check before taking any new medication.
Risk Details
Imagine you’re on dofetilide to keep your heart beating normally after atrial fibrillation. You’ve been stable for months. Then, you get heartburn. You reach for cimetidine - the old-school acid reducer you’ve used for years. Within days, your heart starts racing. You collapse. You’re rushed to the ER. You’ve just had torsades de pointes, a deadly heart rhythm triggered by a simple, preventable drug mix.
This isn’t a hypothetical. It’s happened. And it happens more often than you think.
What Makes This Interaction So Dangerous?
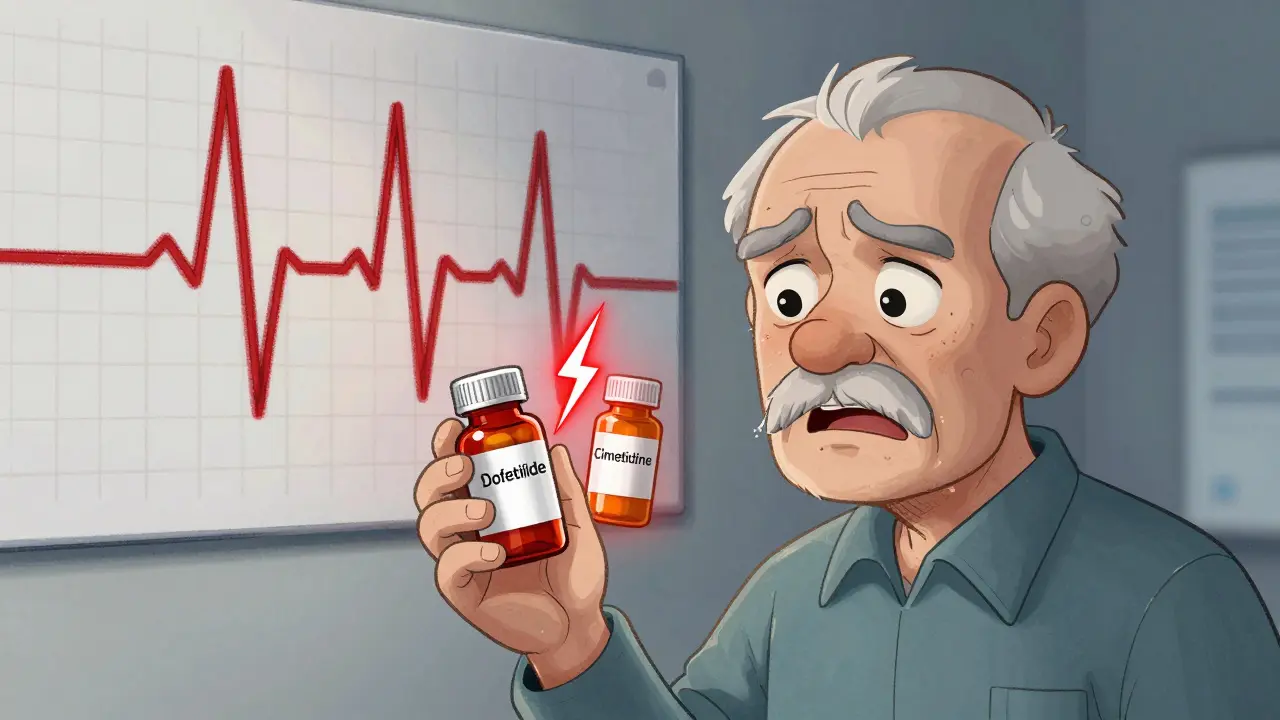
Dofetilide (brand name Tikosyn) is a powerful antiarrhythmic drug. It’s used to restore and maintain normal heart rhythm in people with atrial fibrillation or flutter. But it’s not forgiving. It has a razor-thin safety margin. Too much in your bloodstream, and your heart’s electrical system goes haywire. The result? A prolonged QT interval on your ECG - and a high chance of torsades de pointes, a chaotic, life-threatening rhythm that can turn into sudden cardiac arrest.
Cimetidine (Tagamet) is an H2 blocker. It reduces stomach acid. Sounds harmless, right? But cimetidine doesn’t play nice with kidneys. While most H2 blockers like famotidine or ranitidine are cleared by the liver, cimetidine blocks a specific kidney transport system called the renal cation exchange pathway. That’s the same system your body uses to flush out dofetilide - unchanged - through urine.
When cimetidine shuts down that pathway, dofetilide doesn’t leave your body. It builds up. Studies show plasma levels of dofetilide can spike by 50% to 100% within 24 hours of taking cimetidine. That’s not a minor bump. That’s enough to push a safe dose into the danger zone.
The Numbers Don’t Lie
Let’s look at real data:
- On its own, dofetilide causes significant QT prolongation in 3-5% of patients.
- When taken with cimetidine? That jumps to 12-18%.
- The relative risk of QT prolongation is 4.2 times higher with this combo.
- Between 2010 and 2022, the FDA’s adverse event database recorded 23 confirmed cases of torsades de pointes directly tied to this interaction.
- Cardiologists report that 12-15% of unexpected torsades cases in dofetilide patients involve hidden cimetidine use.
One 72-year-old man on stable dofetilide 500 mcg twice daily started cimetidine 400 mg twice daily for heartburn. Three days later, he went into torsades de pointes. He needed emergency cardioversion and ICU care. Another woman took a single 300 mg dose of cimetidine for a bad bout of acid reflux - and collapsed with polymorphic ventricular tachycardia.
Why Cimetidine? Why Not Other Acid Reducers?
This isn’t true for all H2 blockers. Famotidine (Pepcid) and ranitidine (Zantac) don’t block the renal cation transporter. They’re cleared differently. Clinical trials show famotidine has no meaningful effect on dofetilide levels. Ranitidine, even though it’s mostly off the market now, had the same clean profile.
Cimetidine is the outlier. It’s the only H2 blocker that does this. And it’s not just about dose. Even standard doses - 400 mg twice daily - are enough to cause the problem. That’s why the FDA, the American College of Cardiology, and the European Heart Rhythm Association all say: Contraindicated.
It’s not a "use with caution" warning. It’s a hard stop. The Hemiya Drug Interaction Severity Scale gives this combo a Level 1 rating - the highest risk category. No exceptions.
What Should You Do Instead?
If you’re on dofetilide and need acid control, you have safe options:
- Famotidine (Pepcid): Up to 40 mg twice daily. No interaction. First choice.
- Proton pump inhibitors (PPIs): Omeprazole, esomeprazole, pantoprazole. All safe. No effect on dofetilide.
- Antacids: Tums, Rolaids. Fine for occasional use.
There’s no need to risk your life for heartburn relief. These alternatives work just as well - and they won’t turn your heart into a ticking bomb.
What If You’ve Already Taken Both?
If you’ve accidentally taken cimetidine while on dofetilide, don’t panic - but act fast.
- Stop cimetidine immediately.
- Get an ECG. Check your QT interval. If it’s over 440 ms (or 500 ms if you have bundle branch block), you’re at high risk.
- Check your potassium. Low potassium (below 3.6 mmol/L) makes everything worse. Aim for 4.0-5.0 mmol/L.
- Call your cardiologist. Do not wait for symptoms.
If you’re being switched from cimetidine to another acid reducer, your doctor should delay restarting dofetilide for at least 10 days - five half-lives - to let cimetidine fully clear. Then, recheck your QT interval before restarting.
How Hospitals Are Stopping This Before It Happens
This interaction used to be a common mistake. In 2015, nearly 9% of patients on dofetilide were accidentally prescribed cimetidine. Today? It’s down to 1.2%.
Why? Because hospitals got smart.
- Epic and Cerner EHR systems now block the prescription. If a doctor tries to order cimetidine for someone on dofetilide, the system shuts it down. A pop-up says: "CONTRAINDICATED. TORSADES DE POINTES RISK." To override, you need a cardiologist’s signature.
- Pharmacists run automated checks before dispensing. If cimetidine shows up on a dofetilide patient’s list, the pharmacy calls the prescriber.
- AI tools now predict these interactions 72 hours before they happen - scanning medication lists, lab results, and even OTC purchases flagged in patient portals.
It’s not just technology. It’s culture. Cardiology departments now train nurses, pharmacists, and even front desk staff to ask: "Are you taking Tagamet?" before starting dofetilide.
Why This Matters More Than Ever
There are over 6 million Americans with atrial fibrillation. About 1 in 5 are on rhythm-control drugs like dofetilide. And most of them are on 6 or more other medications - blood thinners, beta-blockers, diuretics, statins.
Polypharmacy is the new normal. But some interactions are silent killers. The dofetilide-cimetidine combo is one of them. It’s predictable. It’s well-documented. It’s avoidable.
And yet, it still happens. In nursing homes. In ERs. In clinics where old prescriptions linger. In patients who buy cimetidine over the counter because they don’t think it’s "real medicine."
The American Geriatrics Society lists this combination as one of the most inappropriate for older adults. Why? Because kidneys slow down with age. Dofetilide builds up faster. Cimetidine lingers longer. The risk isn’t just higher - it’s exponential.
Bottom Line: No Exceptions
There is no safe dose of cimetidine with dofetilide. Not 400 mg. Not 200 mg. Not one pill. Not for two days. Not for heartburn. Not for ulcers. Not even if you think you’re "just taking it once."
This isn’t a gray area. It’s black and white. The evidence is overwhelming. The consequences are fatal. The alternatives are safe and effective.
If you’re on dofetilide - and you’re taking cimetidine - stop it now. Talk to your doctor. Switch to famotidine or a PPI. Your heart will thank you.
If you’re a clinician - check every patient’s medication list. Ask the question. Block the script. Save a life.
Can I take famotidine instead of cimetidine while on dofetilide?
Yes. Famotidine (Pepcid) is the preferred alternative. Unlike cimetidine, it does not inhibit the kidney transport system that clears dofetilide. Studies show no significant change in dofetilide levels when taken with famotidine, even at full doses of 40 mg twice daily. It’s safe, effective, and widely available.
How long does cimetidine stay in the body after stopping?
Cimetidine has a half-life of about 2 hours in healthy adults, but its inhibitory effect on renal transport lasts longer - up to 24-48 hours. However, because it can cause prolonged changes in dofetilide clearance, guidelines recommend waiting at least 10 days (five half-lives of dofetilide) before restarting dofetilide after stopping cimetidine. This ensures the kidney transport system fully recovers.
Is cimetidine still commonly prescribed today?
Not as much as it used to be. In the 1990s, over 28 million prescriptions were written annually. By 2022, that number dropped to about 1.2 million. Most of those are now for short-term use in institutional settings like hospitals or nursing homes, where older records or habits persist. But it’s still available over the counter, which is why patient education remains critical.
Can other drugs cause the same interaction as cimetidine?
Yes. Dofetilide interacts with several other drugs that block the same kidney transporter: verapamil, trimethoprim (in Bactrim), ketoconazole, and some antifungals. Even some antibiotics and heart medications can raise dofetilide levels. Always review your full medication list with your cardiologist before starting any new drug - even if it’s "just a pill for a cold."
What should I do if I experience palpitations or dizziness while on dofetilide?
Stop taking any new medications, including OTC products like cimetidine, and get an ECG immediately. Dizziness, fluttering in your chest, or fainting could be signs of QT prolongation or torsades de pointes. Don’t wait. Call your doctor or go to the ER. Early detection saves lives.
For patients on dofetilide, medication safety isn’t about convenience - it’s about survival. This interaction is preventable. It’s known. It’s avoidable. Don’t let a simple heartburn pill become your last.
15 Responses
OMG I just read this and my heart stopped 😱 I’ve been on dofetilide for 2 years and I used to grab Tagamet every time I had heartburn… I just threw out my last bottle. Thank you for saving my life with this post 💖
i read this and i just cried
my uncle died from something like this
no one told him
he just took tagamet for his stomach
and then he was gone
why do we let people die like this
THIS IS A BIG PHARMA COVERUP!!
They knew cimetidine was dangerous for 30 years but kept it on shelves so they could sell more expensive PPIs!!
Look at the timeline-right after Pepcid got patent-protected, Tagamet got quietly demonized!
And don’t get me started on how the FDA is owned by Big Pharma!!
They want you dependent on $200/month PPIs while letting you die on $5 cimetidine!!
It’s all about profit, not your life!!
They’ll let you go into torsades so you’ll need a pacemaker, then a stent, then a transplant!!
Wake up people!!
They’re poisoning us with bureaucracy!!
And don’t trust your doctor-they’re paid by the drug companies!!
I’ve seen the documents!!
It’s all coded in the EHR alerts!!
They call it ‘contraindicated’ but they mean ‘profitable’!!
STOP TRUSTING THE SYSTEM!!
This is the kind of post that makes me believe in the power of medical education.
Every single person who reads this and switches to famotidine just saved their own life.
You don’t need a PhD to understand this-you just need to listen.
And if you’re a clinician reading this? Thank you for paying attention.
This is how we change outcomes.
Not with fancy tech, but with simple, clear, honest communication.
Keep sharing this.
Someone’s mother, father, sibling, or friend is reading this right now.
And they’re alive because you wrote it.
my grandma took tagamet for years
she never knew it could kill her
she’s fine now she switched to pepcid
thank you for this
I’m a nurse in a cardiac unit and I’ve seen this exact scenario play out three times.
Always the same: patient on dofetilide, takes cimetidine for heartburn, collapses in the hallway.
Always, always, always they say, ‘But it’s just an antacid.’
It’s not just an antacid.
It’s a silent killer.
I keep a printed copy of this interaction list taped to the med cart.
Every shift.
Every patient.
Ask the question.
It takes 10 seconds.
It might save a life.
Let me tell you something-if you’re on dofetilide and you’re still using cimetidine, you’re playing Russian roulette with your heart.
And the gun isn’t loaded once.
It’s loaded every single time you take it.
There’s no ‘maybe’ here.
No ‘I’ll just take it once.’
One pill. One chance.
And your heart doesn’t get a second try.
Switch now.
Don’t wait for the dizzy spell.
Don’t wait for the collapse.
Do it today.
Your future self will thank you.
It is profoundly regressive that laypersons are still permitted to self-administer cimetidine without clinical oversight, particularly in an era where pharmacogenomic risk stratification is not only feasible but routine.
One must question the ethical integrity of a healthcare system that permits the continued OTC availability of a drug with a known, quantifiable, and lethal interaction profile.
The fact that this interaction is not universally flagged in automated pharmacy systems speaks to a systemic failure of governance.
One cannot help but wonder whether this is a consequence of regulatory capture or simply bureaucratic inertia.
Either way, it is unacceptable.
And yet, here we are.
People are dying because we chose convenience over competence.
And for that, we are all complicit.
i just found out my neighbor died last week from this and i felt so bad because i told her to try tagamet for her heartburn last month
i didn't know
i'm so sorry
she was 71 and loved baking cookies
she had atrial fibrillation too
and i just told her to take it like i did
now i can't eat cookies anymore
every time i smell them i think of her
and i cry
please everyone just stop using tagamet if you're on any heart rhythm medicine
i promise you it's not worth it
even if you think you're fine
you're not
Let’s be real-this is just another example of how medicine has become a grotesque parody of itself.
We’ve got AI systems blocking cimetidine prescriptions while ignoring the fact that 70% of patients on dofetilide are also on diuretics that cause hypokalemia.
But no one talks about that.
Because fixing electrolyte imbalances requires clinical judgment.
And judgment doesn’t scale.
Algorithms do.
So we automate the low-hanging fruit-the easy, textbook interaction-and call it a win.
Meanwhile, the real killers-polypharmacy, renal decline, silent hypokalemia-are left to fester.
This isn’t prevention.
This is performative safety.
And we’re all just actors in the theater of medical theater.
In India, we call this ‘dawa ka jadoo’-medicine magic.
People think if it’s sold over the counter, it’s safe.
But your heart doesn’t care where you bought it.
It only cares what’s in your blood.
This post? It’s not just info.
It’s a lifeline.
Share it with your uncle who still takes Tagamet.
Share it with your cousin who just got a new heart rhythm script.
One message could save a family.
I used to think all acid meds were the same.
Now I know better.
Thank you for making this so clear.
I’ll never take cimetidine again.
And I’ll ask my doctor before trying anything new.
It’s not about being paranoid.
It’s about being smart.
Oh my GOD, I can't believe people are still using this!!
It's not just dangerous-it's INSENSITIVE!!
Who lets their grandma take Tagamet?!
It's like giving someone a loaded gun and saying 'be careful'!!
And don't even get me started on how lazy doctors are!!
They just prescribe and forget!!
And now people are DYING because no one checked!!
It's disgusting!!
My cousin almost died from this and the pharmacy didn't even warn her!!
They just handed her the bottle!!
WHO IS RESPONSIBLE HERE?!
THE PHARMACY?!
THE DOCTOR?!
THE PATIENT?!
NO ONE!!
EVERYONE IS TO BLAME!!
It’s strange, isn’t it?
We spend billions on AI that predicts heart attacks, yet we still let people die from a 50-year-old drug interaction.
Technology doesn’t fix ignorance.
It just hides it behind pop-ups.
What if the real problem isn’t cimetidine?
What if it’s that we’ve stopped teaching patients how to think about their own bodies?
We give them pills and instructions.
We don’t give them questions.
What does this do?
Why does this matter?
Who am I trusting?
Maybe the most dangerous drug isn’t cimetidine.
Maybe it’s apathy.
Switched to famotidine last week. No more heartburn. No more fear. This post saved me. Thank you.