When your muscles suddenly feel heavy, your arms won’t lift, or climbing stairs becomes a struggle, it’s easy to blame aging or laziness. But if this weakness comes with a purple rash on your eyelids or unexplained fatigue that doesn’t go away, it could be something far more serious: dermatomyositis or polymyositis. These are rare autoimmune diseases where your immune system turns against your own muscles-sometimes even your skin-and causes chronic inflammation that can steal your strength, your independence, and your quality of life.
What Exactly Are Dermatomyositis and Polymyositis?
Both dermatomyositis (DM) and polymyositis (PM) are types of inflammatory myopathies-diseases that cause muscle inflammation. They’re not the same, but they’re closely related. Polymyositis affects only the muscles, while dermatomyositis adds a distinctive skin rash to the mix. Neither is contagious, nor caused by injury or overuse. They’re autoimmune: your body’s defense system, meant to fight infections, mistakenly attacks healthy muscle tissue.
Polymyositis typically shows up in adults between 30 and 60, with women being two to three times more likely to develop it than men. Dermatomyositis has a bimodal pattern-it can strike children between 5 and 15, or adults in their 40s and 50s. In both cases, the weakness is symmetrical, meaning both sides of the body are affected equally. You’ll notice trouble rising from a chair, lifting your arms above your head, or even swallowing food.
The hallmark of dermatomyositis is the rash. A violet-colored swelling on the eyelids-called a heliotrope rash-is one of the clearest signs. You might also see red, scaly patches on your knuckles, elbows, knees, or neck. These rashes aren’t just cosmetic; they’re a clue that your immune system is active in the skin and muscles.
How Doctors Diagnose These Conditions
Diagnosing these diseases isn’t quick. On average, patients see four different doctors and wait over two years before getting a correct diagnosis. That’s because symptoms overlap with fibromyalgia, thyroid disorders, or even normal aging. Many are told they’re just "tired" or "stressed." But there are specific tests that point to the real problem.
First, blood tests check for elevated creatine phosphokinase (CPK), a muscle enzyme that leaks into the blood when muscle fibers are damaged. In active disease, CPK levels can be five to ten times higher than normal. Other markers like ESR and CRP show general inflammation. Autoantibodies-like anti-Jo-1 or anti-Mi-2-are also tested; these are like fingerprints of the immune system’s attack, and they help distinguish between subtypes.
An electromyography (EMG) measures electrical activity in your muscles. In both DM and PM, it shows abnormal patterns-short, low-amplitude signals and spontaneous firing-signs that muscle fibers are inflamed and misfiring. An MRI can reveal swelling and inflammation deep in the muscles, helping doctors decide where to biopsy.
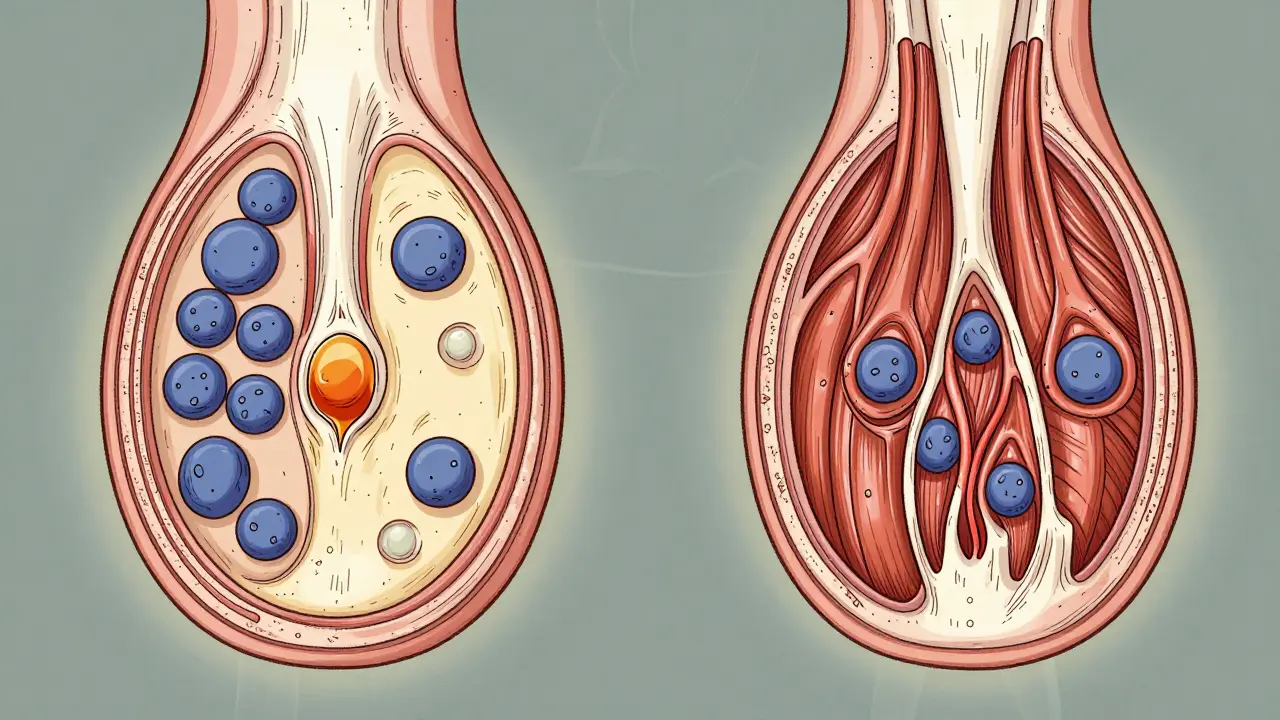
But the gold standard is a muscle biopsy. A small sample of muscle, usually from the thigh or upper arm, is examined under a microscope. In polymyositis, you’ll see immune cells (T cells) clustering around muscle fibers that aren’t dead yet. In dermatomyositis, the damage looks different: muscle fibers at the edges of muscle bundles shrink (perifascicular atrophy), and small blood vessels are surrounded by immune cells. This difference isn’t just academic-it tells doctors how the disease works and how best to treat it.
Why the Difference Between DM and PM Matters
It’s not just about skin rashes. The underlying immune mechanisms are different. Polymyositis is driven by T cells-immune soldiers that directly invade and destroy muscle fibers. Dermatomyositis, on the other hand, is more like a traffic jam of antibodies and B cells attacking blood vessels that feed the muscle. This explains why skin is involved: those blood vessels run through the skin too.
This distinction also affects cancer risk. About 20% of adults with dermatomyositis develop cancer within a few years of diagnosis-especially ovarian, lung, or colon cancer. That’s why doctors recommend full cancer screening at diagnosis: chest CT, pelvic ultrasound, mammogram, colonoscopy. Polymyositis doesn’t carry the same cancer link. Missing this could cost someone their life.
Another key difference? Lung involvement. Up to 40% of dermatomyositis patients develop interstitial lung disease-scarring in the lungs that causes shortness of breath. It’s often silent at first. Regular lung function tests are part of routine care for DM patients. Polymyositis rarely affects the lungs this way.
How These Diseases Are Treated Today
There’s no cure, but treatment can restore strength and prevent long-term damage-if it starts early. The goal isn’t just to reduce symptoms; it’s to stop the immune system from eating away at muscle tissue.
First-line treatment is always corticosteroids. Prednisone is the most common, usually started at 1 mg per kilogram of body weight daily-about 40 to 60 mg for an average adult. This quickly reduces inflammation. Within 4 to 8 weeks, muscle strength often improves, and CPK levels drop. But steroids come with a heavy price: weight gain, insomnia, high blood sugar, bone thinning, and cataracts. Half of long-term users develop osteoporosis. That’s why doctors pair steroids with calcium, vitamin D, and sometimes bisphosphonates to protect bones.
Because steroids alone aren’t enough for most people, second-line drugs are added early. Methotrexate is the most common-it’s an old drug, but it works. Azathioprine and mycophenolate mofetil are alternatives. For patients who don’t respond, intravenous immunoglobulin (IVIG) is used. It’s expensive and requires weekly infusions, but for refractory dermatomyositis, it can be life-changing. One patient on Reddit reported his CPK dropped from 8,200 to 450 after adding methotrexate to his steroid regimen.
Newer options are emerging. JAK inhibitors like tofacitinib, originally used for rheumatoid arthritis, showed 65% improvement in skin rashes and 52% improvement in muscle strength in a 2023 trial for dermatomyositis. Abatacept, which blocks T-cell activation, is being tested in polymyositis with promising early results. Rituximab, which targets B cells, has helped 60-70% of patients who didn’t respond to other treatments.
Rehabilitation Is Just as Important as Medication
Medication stops the attack-but it doesn’t rebuild what’s been lost. That’s where physical therapy comes in. Starting exercise within two weeks of diagnosis is critical. Too little movement leads to permanent muscle wasting. Too much can make inflammation worse.
Therapy is tailored: low-resistance, high-repetition exercises-like light weights, resistance bands, or swimming-help rebuild strength without triggering flare-ups. A 2022 study from the Hospital for Special Surgery found that patients who stuck with a structured program improved their functional capacity by 35-45% in just six months. Many regained the ability to walk without a cane, climb stairs, or hold a grandchild.
Swallowing problems affect up to 30% of patients. Speech therapists help with safe swallowing techniques and recommend softer diets. In severe cases, a feeding tube might be needed temporarily. Fatigue is another hidden burden-68% of patients report it as their biggest challenge. Pacing, rest, and sleep hygiene are part of daily management.

What Life Looks Like After Diagnosis
Prognosis has improved dramatically. In the 1970s, only half of patients survived ten years. Today, over 80% do. Early treatment is the biggest factor. Patients who start therapy within six months of symptoms have an 80% chance of reaching low disease activity or remission.
But it’s not a straight path. Flares happen. Stress, infections, or skipping meds can trigger them. About 41% of patients report moderate to severe side effects from steroids-weight gain is the most common, reported by 82% of those affected. Insomnia, mood swings, and diabetes are real concerns.
Access to care is another hurdle. There are only about 5,800 rheumatologists in the U.S. for 58 million people with autoimmune diseases. Getting a specialist appointment can take months. Insurance often delays approval for second-line drugs-on average, 17 days per request. Many patients pay out of pocket for IVIG or newer drugs because they can’t wait.
Still, there’s hope. Patient support groups, like the Myositis Association, report that 74% of those who engaged in physical therapy saw meaningful improvement. Education matters: learning to track symptoms, recognize flares, and communicate with your care team reduces hospital visits by 22%.
What’s Next for Treatment and Research
Research is accelerating. In June 2023, the European League Against Rheumatism updated diagnostic criteria to include myositis-specific antibodies (MSAs) as key markers. This means faster, more accurate diagnoses-potentially cutting delays by 30-40%.
There are now over a dozen active clinical trials testing new drugs, including biologics that target specific immune pathways. The focus is shifting from broad immunosuppression to precision medicine: matching the right drug to the right antibody profile.
Meanwhile, the market for myositis treatments is growing-projected to hit $2.1 billion by 2029. But only three drugs are FDA-approved for dermatomyositis, and none for polymyositis. Most treatments are used off-label. That’s why patient advocacy is so important. Without voices pushing for research funding and faster drug approvals, progress stalls.
If you’re living with this, you’re not alone. The path is long, but it’s not hopeless. With the right team-rheumatologist, physical therapist, nutritionist, and support group-you can regain control. Muscle strength can return. Rashes can fade. Life can get better.
Can dermatomyositis or polymyositis be cured?
No, there is no cure for either condition. But with early, aggressive treatment, many patients achieve remission or low disease activity. Muscle strength can improve significantly, and symptoms can be managed long-term with medication, physical therapy, and regular monitoring.
Is dermatomyositis linked to cancer?
Yes, about 20% of adults diagnosed with dermatomyositis develop cancer within the first few years, especially ovarian, lung, or gastrointestinal cancers. That’s why full cancer screening-like CT scans, mammograms, and colonoscopies-is recommended at diagnosis. Polymyositis does not carry this same risk.
How long does it take to diagnose these diseases?
On average, it takes 2 to 3 years and visits to 4 or more doctors before a correct diagnosis is made. Symptoms are often mistaken for fibromyalgia, thyroid issues, or normal aging. Blood tests, EMG, MRI, and muscle biopsy are needed to confirm the diagnosis.
What are the most common side effects of steroid treatment?
Long-term steroid use causes weight gain in 82% of affected patients, insomnia in 67%, osteoporosis in 30-50%, high blood sugar or diabetes in 15-30%, and cataracts in 20-40%. Doctors usually prescribe calcium, vitamin D, and bone-strengthening drugs to reduce these risks.
Can exercise help with muscle weakness from these diseases?
Yes-when done correctly. Low-resistance, controlled exercise like swimming, resistance bands, or light weight training improves muscle strength by 35-45% in six months. Physical therapy must start early and avoid overexertion, which can worsen inflammation. Most patients who stick with therapy regain daily function like climbing stairs or lifting objects.
Are there new treatments on the horizon?
Yes. JAK inhibitors like tofacitinib are showing strong results for skin and muscle symptoms in dermatomyositis. Abatacept and rituximab are being tested in polymyositis. New classification criteria now include specific autoantibodies, which help match patients to targeted therapies faster. Clinical trials are expanding, offering hope for more effective, less toxic treatments in the next few years.

11 Responses
So let me get this straight - we’re giving people steroids that turn them into moon-faced, insomnia-ridden zombies… and calling it a win? 🙄 At least tell me the cancer screening is covered by insurance. Oh wait - it’s not. Classic.
It’s wild how medicine treats inflammation like a villain to be crushed - when really, it’s just a confused alarm system. The body isn’t broken. It’s screaming because it doesn’t know how to stop. Maybe we need to listen more, and blast less.
I love how this post breaks down the science without making you feel dumb. 😊 I’ve got a friend with DM and she’s been on IVIG for a year - it’s expensive as hell, but she can finally pick up her dog again. Small victories, right? 🌱
Honestly, if you’re not on a biologic by year one, you’re just wasting time. I mean, prednisone? In 2024? That’s like treating sepsis with aspirin. And don’t even get me started on how the US healthcare system treats autoimmune patients like second-class citizens. 😒
The pathophysiology is unequivocally Th1/Th17-driven with IFN-α signatures in DM, whereas PM exhibits CD8+ T-cell cytotoxicity - yet clinicians still conflate them. This is why we have 2-year diagnostic delays. We need molecular phenotyping, not just EMG and CPK. And stop calling it 'fatigue' - it's myopathic exhaustion with systemic cytokine dysregulation.
So the immune system’s basically playing Jenga with your muscles, and the doctors are the ones holding the tweezers trying to pull out the right block without the whole tower collapsing? I mean… that’s either brilliant or terrifying. Or both. 😅
Anyone else notice the study from HSS only included patients who already had access to PT? What about the ones in rural areas? Or without insurance? The data’s pretty, but it’s not real life.
Thank you for writing this. In Nigeria, many think it's witchcraft or punishment. I showed this to my cousin - she cried. Now she’s seeing a doctor. 🙏
It’s astonishing how much progress has been made - yet so many still suffer in silence. I’ve seen it firsthand. Please, if you’re reading this and you’re undiagnosed: keep pushing. And if you’re a clinician: listen. Really listen.
CPK? EMG? LOL. I saw a TikTok that said it’s all just gluten. I’m gonna try keto.
They’re hiding the truth - this is all a Big Pharma plot to sell drugs. The real cure? Sunlight + magnesium + avoiding 5G towers. And why are they screening for cancer? Because they want you scared. 😡🔥