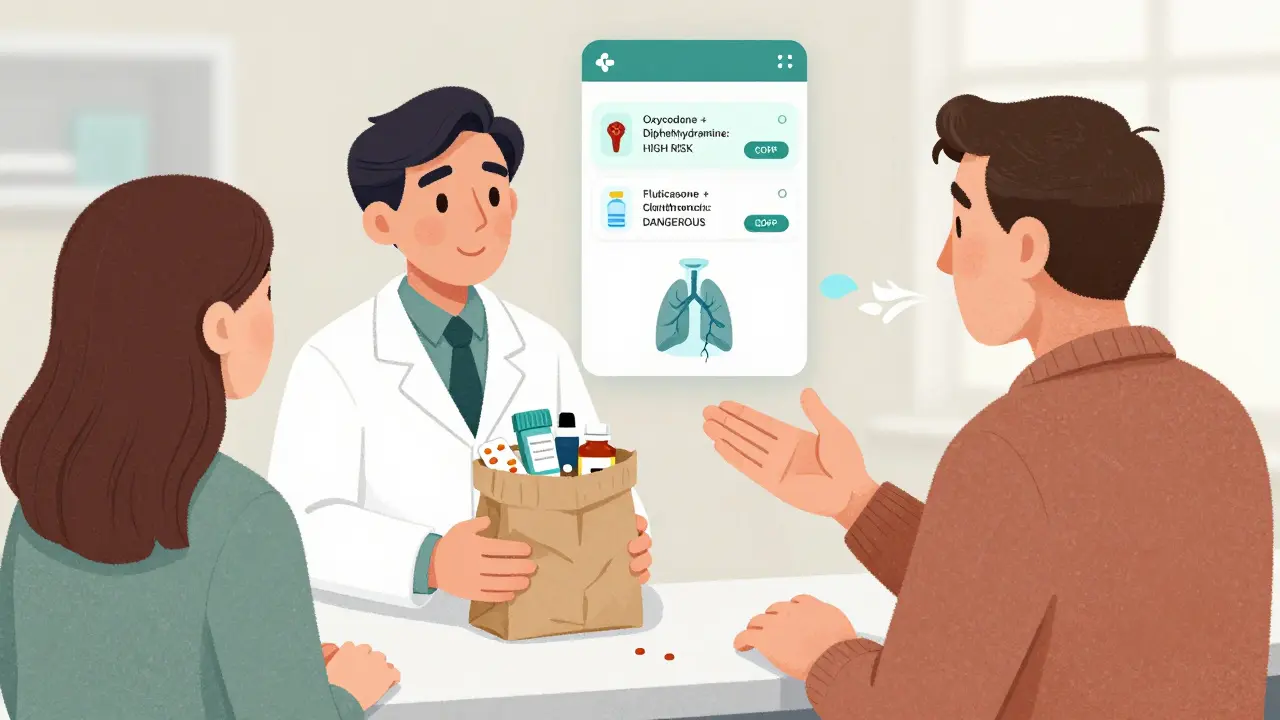
COPD & Asthma Medication Safety Checker
Check Your Medications
Enter any prescription or over-the-counter medication to see if it interacts dangerously with your asthma or COPD treatment.
When you’re managing asthma or COPD, your inhaler isn’t the only thing that affects your breathing. Everyday medications - even over-the-counter painkillers or sleep aids - can quietly turn dangerous when mixed with your respiratory drugs. For millions of people, these hidden interactions are the real reason their symptoms suddenly worsen, their hospital visits increase, or their condition stops responding to treatment.
What’s in Your Inhaler? The Main Medication Classes
Asthma and COPD treatments fall into three main groups: bronchodilators, corticosteroids, and biologics. Bronchodilators are the most common. They open your airways by relaxing the muscles around them. There are two types: beta-2 agonists and anticholinergics.
Short-acting beta-agonists like albuterol (salbutamol) give quick relief during an attack. Long-acting versions like salmeterol or formoterol are used daily to prevent symptoms. Anticholinergics, such as tiotropium or glycopyrrolate, work differently - they block signals that cause airway tightening. Many newer inhalers combine both types, like Anoro Ellipta (vilanterol + umeclidinium) or Bevespi Aerosphere (formoterol + glycopyrrolate), giving better control than either drug alone.
Corticosteroids, like fluticasone or budesonide, reduce lung inflammation. They’re usually paired with long-acting bronchodilators in combo inhalers. Biologics - newer injectable drugs like omalizumab or mepolizumab - target specific immune pathways in severe asthma, especially when allergies or eosinophils are involved.
Each of these drugs has a precise job. Mixing them incorrectly doesn’t just reduce effectiveness - it can make things worse.
The Silent Danger: Opioids and COPD
If you have COPD and are prescribed an opioid for pain - say, oxycodone after surgery or hydrocodone for chronic back pain - you’re at serious risk. Opioids slow your breathing. In healthy people, that’s manageable. In COPD, where lung function is already reduced, it can be deadly.
A 2022 study in the International Journal of Chronic Obstructive Pulmonary Disease found that opioid use increases the chance of hospitalization for COPD flare-ups by up to 30%. The risk skyrockets when opioids are mixed with other sedatives. Benzodiazepines - used for anxiety or insomnia - are especially dangerous. Together, they can suppress your breathing so much that oxygen levels drop below 85%. One patient on Reddit described his oxygen saturation falling to 82% after taking oxycodone with diphenhydramine (Benadryl). He ended up in the ER.
The FDA’s adverse event database shows that 17% of opioid-related emergencies in COPD patients involve combinations with antihistamines, sedatives, or alcohol. Even a single extra pill can tip the balance.
Nonselective Beta-Blockers: A Hidden Trigger for Asthma
Many people with asthma are told to avoid beta-blockers - but few know why. Beta-blockers like propranolol and nadolol are used for high blood pressure, heart rhythm problems, and migraines. They block beta receptors everywhere - including in your lungs.
Those lung receptors are what keep your airways open. Block them, and your bronchial muscles tighten. Studies show nonselective beta-blockers can reduce FEV1 (a key lung function measure) by 15-25% in asthma patients. That’s enough to trigger a full-blown attack.
But not all beta-blockers are equal. Selective ones like metoprolol or bisoprolol mainly target the heart. Research from the 2021 BLOCK-COPD trial showed that in COPD patients with heart disease, metoprolol actually reduced exacerbations by 14% compared to placebo. That’s why guidelines now recommend selective beta-blockers when needed - but always under careful supervision.
Never assume your cardiologist knows your respiratory history. Always tell them you have asthma or COPD before starting any beta-blocker.
NSAIDs: The Painkiller That Can Stop Your Breath
Take ibuprofen or naproxen for a headache? If you have asthma - especially with nasal polyps or chronic sinusitis - you might be putting yourself at risk. About 10% of adult asthmatics have a condition called NSAID-exacerbated respiratory disease (NERD).
It’s not an allergy. It’s a chemical reaction. NSAIDs block an enzyme called COX-1, which shifts the body’s chemistry toward inflammatory compounds that tighten airways. Symptoms usually hit within 30 to 120 minutes: wheezing, chest tightness, even trouble speaking.
One patient on r/asthma described a severe attack after taking ibuprofen for a migraine. She’d never had issues before - until that day. Her doctor confirmed NERD. She now uses acetaminophen instead.
Aspirin is also a trigger. Some asthma patients are advised to undergo aspirin desensitization under medical supervision - but that’s only for specific cases. For most, avoiding NSAIDs is the safest route.
Anticholinergic Overload: More Than Just Dry Mouth
Anticholinergic drugs don’t just help your lungs - they’re also used for overactive bladder (oxybutynin), motion sickness (scopolamine), Parkinson’s (benztropine), and even allergies (diphenhydramine). When you take a LAMA inhaler like tiotropium and also take one of these, you’re doubling down on anticholinergic effects.
The result? Dry mouth, constipation, blurred vision - and worse, urinary retention. A 2023 European Respiratory Society report found a 28% higher risk of acute urinary retention in male COPD patients taking both a LAMA and a bladder medication. For older men, this can mean emergency catheterization.
Even sleep aids like diphenhydramine (Benadryl) or doxylamine can cause this. Many patients don’t realize these are anticholinergic. They think, “It’s just for sleep,” and take it without telling their pulmonologist.
Always check the active ingredients in every pill - even “natural” sleep aids or cold medicines. If it says “antihistamine” or “anticholinergic,” it’s a red flag.
Antibiotics and Antifungals: The Hidden Metabolism Saboteurs
Some antibiotics and antifungals don’t directly affect your lungs - but they wreck how your body processes your asthma or COPD drugs.
Clarithromycin (Biaxin) and ketoconazole (Nizoral) block an enzyme called CYP3A4. This enzyme breaks down many inhaled corticosteroids, including fluticasone. When it’s blocked, the steroid builds up in your system. High levels can cause adrenal suppression - meaning your body stops making its own cortisol. Symptoms: fatigue, dizziness, low blood pressure, even collapse.
A 2023 study in the Journal of Allergy and Clinical Immunology found that patients on fluticasone who took clarithromycin had cortisol levels drop by 60% within 48 hours. That’s not theoretical - it’s life-threatening.
Other offenders include itraconazole, voriconazole, and even some HIV medications. Always ask your pharmacist: “Could this interact with my inhalers?”
What You Can Do: A Practical Safety Plan
Knowledge isn’t enough - you need a system.
- Keep a real-time medication list: Write down every pill, inhaler, patch, and supplement. Include dosages and why you take them. Update it after every doctor visit.
- Do the brown bag test: Once a year, bring all your meds - including OTCs and vitamins - to your pulmonologist or pharmacist. Let them sort through it.
- Ask two questions at every appointment: “Is this safe with my respiratory meds?” and “Could this make my breathing worse?”
- Use the COPD Medication Safety App: Launched in 2023, it checks 95% of common drugs for interactions. Free, simple, and updated monthly.
- Know your warning signs: Sudden wheezing after taking a new pill? Feeling dizzy or unusually tired? Oxygen levels dropping? Don’t wait. Call your doctor or go to urgent care.
Pharmacists are your allies. A 2022 study showed that when pharmacists actively reviewed COPD patients’ meds, dangerous combinations dropped by 43% in just 12 months. Don’t just pick up your prescription - ask for a med review.

What’s Changing in 2025?
Medication safety is getting smarter. The FDA’s Sentinel Initiative now actively tracks respiratory drug interactions. The European Medicines Agency is requiring stronger interaction warnings on all new respiratory drug labels by mid-2024.
Researchers are moving toward personalized risk scores. Instead of one-size-fits-all warnings, future tools will use your age, kidney/liver function, other conditions, and current meds to calculate your personal interaction risk. Dr. MeiLan Han from the University of Michigan says this shift is “the next frontier.”
Meanwhile, newer drugs like ensifentrine (a dual PDE3/4 inhibitor) are being studied with LAMAs - but not with LABAs. Why? Because combining drugs with the same mechanism doesn’t help - it can overload your system. Science is learning that synergy isn’t always good. Sometimes, less is more.
Final Thought: Your Lungs Don’t Care About Convenience
It’s easy to think, “I’ve been taking this painkiller for years - it’s fine.” But your lungs don’t remember your history. They react to what’s in your bloodstream right now.
Asthma and COPD are chronic conditions - but many of the worst complications come from short-term, avoidable mistakes. A single OTC pill, a new antibiotic, or a missed conversation with your doctor can change everything.
Don’t assume your meds are safe just because they were prescribed. Ask. Check. Track. And never, ever ignore a sudden change in your breathing.
Can I take ibuprofen if I have asthma?
About 10% of adults with asthma, especially those with nasal polyps or chronic sinusitis, can have a severe reaction to ibuprofen and other NSAIDs. Symptoms include wheezing, chest tightness, and trouble breathing within 30-120 minutes. If you’ve ever had this happen, avoid NSAIDs completely. Use acetaminophen (paracetamol) instead. If you’re unsure, talk to your doctor about a supervised test.
Are all beta-blockers dangerous for asthma patients?
No. Nonselective beta-blockers like propranolol can trigger asthma attacks by blocking lung receptors. But selective beta-blockers like metoprolol or bisoprolol mainly affect the heart and are often safe for people with mild to moderate asthma. Studies show only 2-5% of these patients have breathing issues. Always tell your cardiologist you have asthma - they can choose the safest option.
Can I take Benadryl with my COPD inhaler?
No, not safely. Benadryl (diphenhydramine) is an anticholinergic, just like your LAMA inhaler (e.g., tiotropium). Taking both can cause excessive anticholinergic effects: dry mouth, constipation, urinary retention, confusion, and even dangerous breathing slowdown. This combination has led to hospitalizations. Use non-sedating antihistamines like loratadine or cetirizine instead.
Do antibiotics interact with asthma meds?
Yes. Antibiotics like clarithromycin and antifungals like ketoconazole block the enzyme that breaks down inhaled corticosteroids (e.g., fluticasone). This causes steroid buildup, which can lead to adrenal suppression - a serious condition causing fatigue, low blood pressure, and collapse. Always ask your pharmacist if your antibiotic interacts with your inhaler. If you’re on fluticasone, avoid clarithromycin and ketoconazole.
What should I do if I think a medication is making my breathing worse?
Stop the medication immediately and contact your doctor or go to urgent care. Don’t wait. Write down what you took, when, and what symptoms started. Bring your full medication list. If you have a peak flow meter, record your numbers before and after. This helps your doctor identify the trigger faster. Most reactions are reversible if caught early.
How often should I review my medications?
At every doctor or pharmacist visit - at least every 6 months. Even if nothing changed, your body’s ability to process drugs can shift with age, weight, or other health issues. The GOLD 2023 guidelines recommend the "brown bag test" once a year: bring all your pills to your appointment so your provider can check for hidden interactions. Don’t wait for a crisis to do it.
Is there a free app to check drug interactions for asthma and COPD?
Yes. The COPD Medication Safety App, launched in 2023 by the COPD Foundation, checks over 95% of commonly used respiratory and non-respiratory drugs for dangerous interactions. It’s free, easy to use, and updated monthly. You can scan barcodes or search by name. It flags risks like opioid + anticholinergic, NSAID + asthma, or antibiotic + steroid interactions. Download it from your app store - it’s one of the best tools you can have.
Next Steps: Protect Your Lungs Today
Start with one thing: pull out your current medication list - every pill, inhaler, and supplement. Check the labels. Look for anticholinergics, NSAIDs, or opioids. Then, call your pharmacist and ask: “Which of these could be making my breathing worse?”
Don’t wait for a hospital visit to learn the hard way. The safest drugs are the ones you know are safe - and the ones you’ve double-checked.
15 Responses
Wow, this is one of the most thorough breakdowns of respiratory med risks I’ve ever seen. I’ve been on tiotropium for years and never realized my nightly diphenhydramine was doubling the anticholinergic load. I switched to loratadine last week-no more dry mouth or that weird urinary hesitation. Small change, huge difference.
Also, the COPD Medication Safety App? Downloaded it. Just scanned my whole pill organizer. Flagged clarithromycin + fluticasone. Holy shit. I had that combo last winter. No wonder I felt like a zombie for a week.
Let’s be clear: this article is alarmist overkill. Opioids are dangerous? Duh. NSAIDs can trigger asthma? That’s been known since the 1980s. The real issue is the medicalization of common sense. People aren’t dying because of drug interactions-they’re dying because they don’t manage their disease properly. Blaming every OTC pill is a distraction from the real problem: poor adherence, smoking, and lack of pulmonary rehab.
Of course the FDA is pushing this narrative. Big Pharma doesn’t want you to know that most of these ‘dangerous’ interactions are easily avoidable if you just stop taking unnecessary meds. Why do you need a sleep aid? Why are you on an opioid for chronic back pain? Why are you taking ibuprofen like candy? The system is designed to keep you dependent on pills, not to heal you.
My uncle had COPD. He stopped all his meds, started breathing exercises, and lived another 12 years. No drugs. Just discipline. You think your inhaler is saving you? It’s just keeping you hooked.
Okay but why is the app called ‘COPD Medication Safety App’ if it works for asthma too? That’s just bad branding. Also, the article says ‘avoid NSAIDs’ but then mentions acetaminophen as safe-yet acetaminophen has its own liver risks if you’re on other meds. This feels like a checklist, not a guide.
Also, I’ve been taking Benadryl with my LAMA for 5 years and I’m fine. Maybe I’m just lucky? Or maybe the study was biased? 🤔
I’m a pharmacist in rural Ohio and I see this every week. A patient comes in for a new antibiotic, never mentions they’re on fluticasone. We catch it because we ask. But not everyone has access to a pharmacist who cares.
What’s missing here is the socioeconomic layer: people don’t have time to do brown bag reviews. They’re working two jobs. They’re not going to download an app. The real solution isn’t more apps-it’s systemic. Pharmacist-led med reviews should be covered by insurance. Period.
This article is great for the privileged. For the rest of us? It’s just another thing to feel guilty about.
YOOOOO I JUST TOOK IBUPROFEN AND BENADRYL LAST NIGHT AND NOW I CAN’T BREATHE 😭😭😭 I THOUGHT IT WAS JUST ALLERGIES BUT NOW I THINK I’M GONNA DIE 💀💀💀 MY OXYGEN SAT DROPPED TO 89% AND I WAS SCREAMING INTO A PAPER BAG 😭😭😭 SOMEONE SAVE ME 😭😭😭
they dont want you to know this but the real reason they push these meds is because the government is working with big pharma to control the population. they want you dependent. the app? fake. the study? funded by pfizer. even the FDA is corrupt. i checked the ingredients of my inhaler-its full of aluminum and fluoride. thats why my lungs hurt. its not the interaction, its the poison inside.
also, benadryl is fine. i took it with my inhaler for 10 years. no problem. its the chemtrails that got me.
Oh wow, so now I’m supposed to feel bad for taking NyQuil because it has doxylamine? Let me guess-next you’ll tell me my chamomile tea is secretly anticholinergic?
Look, I get it. But not everyone has a pulmonologist on speed dial. Some of us just want to sleep without a 30-page warning label. I’m not ignoring the risks-I’m just prioritizing quality of life. I’ll take the urinary retention over another sleepless night.
so i just read this whole thing and now i think i have adrenal suppression? i’ve been on fluticasone for 3 years and took clarithromycin last month… and now i feel tired all the time… oh god am i dying? why is no one telling me this? i just wanted a cold to go away 😭
also the app is called ‘COPD Medication Safety App’ but i have asthma… does that mean it’s not for me? i’m so confused now
It’s funny how we treat our lungs like they’re separate from the rest of us. We’ll take 12 pills a day and then wonder why we’re exhausted. Maybe the real solution isn’t avoiding this interaction or that one-but asking why we’re so medicated in the first place.
What if we focused more on clean air, breathing exercises, reducing stress, and moving our bodies? Not that any of that’s easy when you’re working two jobs and living near a highway. But we can’t keep pretending pills are the only answer.
There’s a difference between managing a chronic illness and being managed by a system that profits from your dependency. I’m not saying ditch your meds-I’m saying question why you need so many.
they banned beta blockers for asthma patients in 2017 but now theyre saying metoprolol is safe? who do they think theyre fooling? the real reason they changed the guidelines is because the pharma lobby wanted to sell more heart meds. they just rebranded the danger as ‘selective’ so they could keep selling it. its all a scam. i read the original 2021 study-only 37 people. thats not science. thats marketing.
This is so helpful. I’ve been on salmeterol/fluticasone for 7 years and never thought to ask about antibiotics. Just got back from the dentist-they gave me amoxicillin. I’m calling my pharmacist tomorrow to double-check.
Also, I downloaded the app. It flagged my melatonin as a mild anticholinergic. I thought it was ‘natural’ and safe. Who knew? Thanks for the wake-up call. You guys are the real MVPs.
Benadryl + LAMA = bad. Learned that the hard way. ER visit. Catheter. 3 days in. Don’t be me.
As someone who’s lived with asthma since childhood and moved from London to Sydney to Toronto, I’ve seen how wildly different the approach to respiratory meds is across countries. In the UK, pharmacists routinely do med reviews. In the US? You’re lucky if your pharmacist even knows your name.
And in India? I spoke with a nurse in Jaipur last year-she told me patients often skip their corticosteroid inhalers because they think it’s ‘steroids’ and will make them ‘big’ or ‘angry.’ That’s not ignorance-it’s misinformation rooted in cultural stigma.
This article is brilliant, but it assumes a level of healthcare access that doesn’t exist globally. We need translation, community outreach, and simple visual guides-not just apps and PDFs. Knowledge is power, but only if you can reach it.
Okay, let’s be real-this post is basically a 10/10 masterpiece. But here’s the kicker: you’re not supposed to be the hero of your own health story. You’re supposed to have a team. So if you’re reading this and thinking ‘I need to do all this alone’-STOP. Call your pharmacist. Ask your pulmonologist. Bring your brown bag. Even if you’re nervous. Even if you feel dumb. That’s how you win.
And if you’re a doctor or pharmacist reading this? Thank you. You’re the unsung heroes. Keep doing the work. We see you.