When you’re taking antiviral meds for HIV or hepatitis C, it’s not just about the pill in your hand. What you’re really dealing with is a complex chemical dance inside your body-one that can go wrong if other drugs, supplements, or even food get in the way. Two players in this dance are CYP3A4 and P-glycoprotein (P-gp). They’re not household names, but they control whether your antiviral works, stays in your system too long, or gets flushed out before it can do its job.
What Are CYP3A4 and P-glycoprotein?
CYP3A4 is the most common enzyme in your liver and gut that breaks down drugs. Think of it like a trash compactor for medications. About half of all prescription drugs, including many antivirals, pass through it. If CYP3A4 is slowed down, those drugs build up in your blood. Too much? You risk side effects like liver damage, bleeding, or heart rhythm problems.
P-glycoprotein is a pump that kicks drugs out of your cells. It’s like a bouncer at the door of your intestines and brain. If P-gp is working hard, it pushes antivirals back into your gut before they can be absorbed. If it’s blocked, those same drugs flood into your bloodstream.
These two systems often work together. A drug might be broken down by CYP3A4 and pumped out by P-gp. If both are inhibited, the drug can skyrocket in your system-sometimes by 10 times or more.
Why Ritonavir Changed Everything
In 1996, ritonavir was approved as an HIV protease inhibitor. But doctors noticed something strange: when patients took low doses (100 mg), other HIV drugs worked better. Turns out, ritonavir doesn’t just fight the virus-it shuts down CYP3A4 and P-gp like flipping a switch.
That’s how the “booster” concept was born. Today, ritonavir is rarely used alone. Instead, tiny doses (100 mg) are added to drugs like lopinavir or darunavir to make them last longer and work stronger. But here’s the catch: that same boost makes everything else you take more dangerous.
Studies show ritonavir can increase levels of midazolam (a sedative) by 300-500%. That’s not a typo. One patient on warfarin (a blood thinner) and ritonavir had an INR level over 12-normal is 2-3. They nearly bled to death.
Not All Antivirals Are Created Equal
Some antivirals are heavy hitters when it comes to interactions. Others? Barely a ripple.
- Ritonavir-boosted regimens (like Kaletra or Viekira Pak) are the most problematic. They can raise simvastatin levels by 1,760%. That’s enough to cause muscle breakdown and kidney failure.
- Cobicistat (used in Stribild and Genvoya) is a newer booster. It’s just as strong as ritonavir at blocking CYP3A4-but doesn’t mess with CYP1A2. That means fewer weird side effects, like reduced antidepressant levels.
- Glecaprevir/pibrentasvir (Mavyret) has far fewer interactions. Only 17% of common meds need dose changes, compared to 42% with older combos.
- Sofosbuvir (in Sovaldi, Epclusa) barely touches CYP3A4. But it’s a P-gp substrate. So if you’re on a P-gp blocker like verapamil, your sofosbuvir levels could rise.
That’s why doctors now avoid ritonavir-boosted drugs if you’re on statins, blood thinners, or anti-seizure meds. Newer options like lenacapavir are designed to avoid these pathways entirely. They’re the future.
Hidden Dangers: Supplements, Food, and Herbs
It’s not just prescription drugs that cause trouble. Common stuff you might think is harmless can be deadly with antivirals.
- St. John’s wort-a popular herbal remedy for depression-can slash ritonavir levels by 57%. That’s like skipping your dose for days. Viral rebound can happen fast.
- Grapefruit juice blocks CYP3A4 in your gut. One glass can raise antiviral levels by 23%. That’s why some clinics warn patients: no grapefruit, no pomelos, no Seville oranges.
- Cyclosporine (used after transplants) can cause a 17-fold spike in grazoprevir levels. That combo is outright banned in guidelines.
Even over-the-counter painkillers like ibuprofen can interact. Not because they’re metabolized by CYP3A4, but because they stress the liver-already working overtime to process antivirals.
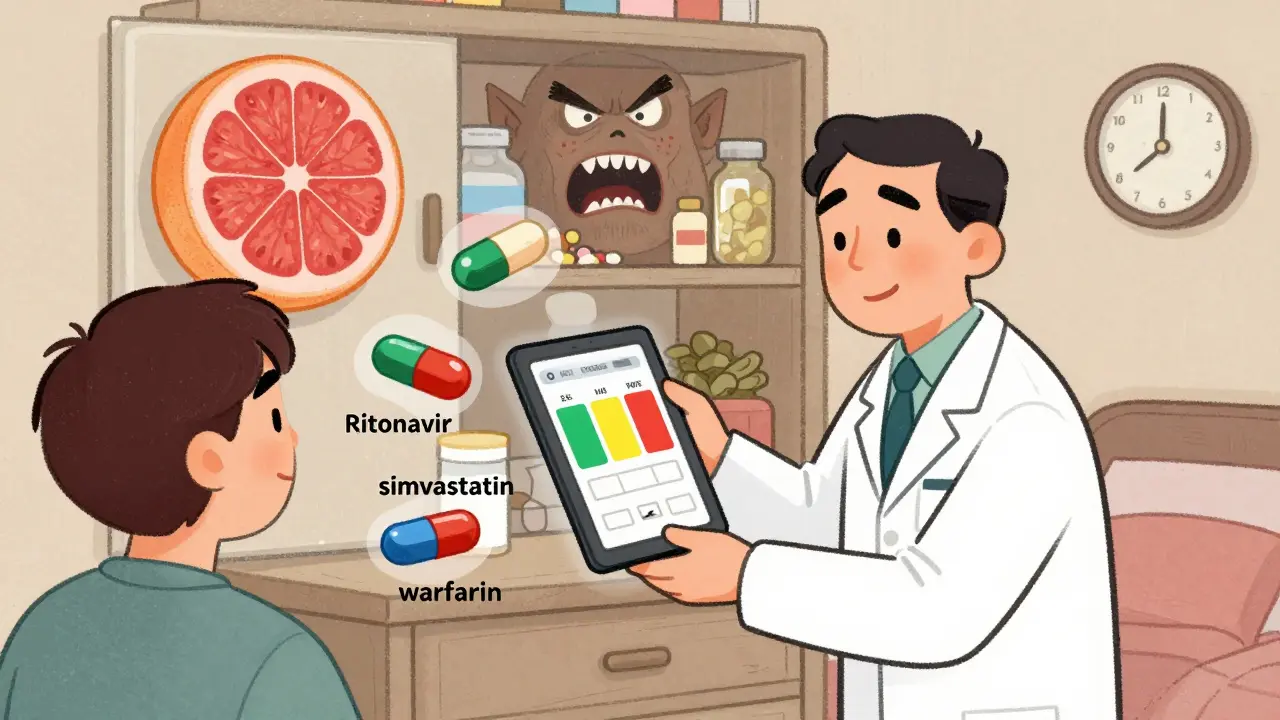
How Doctors Manage This in Real Life
It’s not guesswork. Clinics use tools-real, tested ones.
The University of Liverpool HIV Drug Interactions Checker is free, online, and used in 92% of European HIV clinics. You plug in your meds, and it gives you a color-coded risk level: green (safe), yellow (monitor), red (avoid). It’s updated daily. One study showed using it dropped interaction-related hospitalizations from 18.7% to 5.2% in just a year.
Electronic health records now have built-in alerts. Epic Systems added antiviral interaction checks in 2021. At Mayo Clinic, severe interactions dropped by 31% after implementation.
But tech isn’t enough. Doctors still need to ask the right questions:
- “Are you taking any herbs or supplements?”
- “Have you started anything new in the last month?”
- “Do you drink grapefruit juice?”
Patients often don’t think of these as “medications.” But they’re just as dangerous as pills.
What Patients Are Saying
Reddit threads are full of frustration. One user, u/HIVWarrior, wrote: “My psychiatrist won’t prescribe me anything for anxiety because of my darunavir regimen. It’s like choosing between mental health and viral suppression.”
That’s real. Antivirals can lock you out of common treatments for depression, pain, or heart disease. But it’s not hopeless. A clinician on the American Academy of HIV Medicine forum shared a trick: delay starting blood thinners or antidepressants until after the first month of antiviral therapy. That lets your body adjust to the new drug load.
Another patient, on a regimen with minimal interactions, said: “I can finally take my blood pressure meds and my sleep aid without checking a website every time. It’s life-changing.”
What’s Next?
The field is moving fast. Pharmacogenomics-testing your genes-is becoming part of the standard. If you have the CYP3A5*3/*3 genotype (common in white populations), you process drugs slower. Combine that with ritonavir, and you’re at higher risk for toxicity.
By 2025, nearly 40 million people worldwide will be on antivirals. Most will be older, with multiple chronic conditions. One study found the average HIV patient has 4.7 other health problems. That’s a lot of meds. And every one of them could clash.
The answer isn’t just better drugs. It’s better systems: routine screening, better EHR alerts, patient education, and access to free interaction checkers. Because when you’re taking antivirals, safety isn’t optional. It’s the foundation.
What You Can Do Today
- Make a list of everything you take-prescriptions, supplements, herbs, even occasional painkillers.
- Use the University of Liverpool HIV Drug Interactions Checker (free, no login needed).
- Ask your pharmacist: “Is this safe with my antiviral?” Don’t assume they know.
- If you’re on ritonavir or cobicistat, avoid grapefruit, St. John’s wort, and high-dose fish oil.
- Never start or stop a med without checking interactions first-even if it’s “just” an OTC painkiller.
Antiviral therapy isn’t just about killing the virus. It’s about keeping your whole body safe while you do it. The science is clear. The tools exist. What matters now is using them.

9 Responses
Bro this post is basically a 10-page pharmacology lecture dressed up as a Reddit thread. CYP3A4? P-gp? You talking like you’re explaining quantum physics to your cat. I get it’s important, but most people just want to know if their grapefruit smoothie will kill them. Stop with the jargon and just say: ‘If you’re on antivirals, don’t touch grapefruit, St. John’s wort, or your uncle’s ‘miracle’ herbal tea.’ Done.
The University of Liverpool database is the gold standard. I’ve used it daily for five years in clinical practice. It’s free, accurate, and updated hourly. If your provider isn’t using it, they’re either lazy or unaware. No excuses. Also, cobicistat is not ritonavir 2.0-it’s just better at avoiding CYP1A2 interference. That’s why I switched all my depressed patients to it. Simple. Effective.
Let me ask you something. Who really funds these ‘free interaction checkers’? The pharmaceutical industry? Of course. They want you to believe the system is safe. But what about the 200+ undocumented herbal blends sold in Indian pharmacies? The ones that contain hidden CYP3A4 inhibitors? The ones that don’t even have ingredient labels? The FDA doesn’t track them. Neither does Liverpool. You think this is about safety? No. It’s about control. You’re being trained to trust algorithms, not your own instincts. Wake up.
St. John’s wort ruins everything. I tried it with my darunavir. Got viral load spike in 3 days. My doc said ‘it’s just an herb’ like that’s a free pass. Bro. It’s not. It’s a chemical bomb. Also, why is everyone acting like ritonavir is the devil? It saved my life. The side effects? Yeah, I got them. But I’m alive. So shut up.
So… if I take my antiviral with a glass of grapefruit juice, do I get a free trip to the ER? 🍊🩺😭 I’m just asking for a friend. (It’s me. It’s always me.)
What struck me most isn’t the science-it’s the loneliness. The user who said they can’t take anxiety meds because of their antiviral regimen? That’s not just a drug interaction. That’s a human cost. We talk about viral suppression like it’s the only goal. But what about mental health? Sleep? Quality of life? These drugs don’t exist in a vacuum. They live inside people who have jobs, families, grief, and fear. The tools matter. But so does the humanity behind them.
Let’s get real: ritonavir is the OG drug boss. It doesn’t just boost antivirals-it rewires your entire metabolic ecosystem. I’ve seen people on simvastatin turn into walking jellyfish from rhabdo. One guy’s CK hit 80,000. He didn’t even know what CK was. Now? I don’t even prescribe statins to anyone on ritonavir unless they’ve got a heart attack breathing down their neck. And even then, I switch to pravastatin or rosuvastatin-those don’t dance with CYP3A4. Smart prescribing isn’t about being fancy. It’s about not turning your patient into a science experiment gone wrong.
I appreciate the depth here. It’s rare to see a post that doesn’t just say ‘avoid grapefruit’ but actually explains why. I’ve been on antivirals for 12 years and never knew P-gp was a bouncer. That analogy stuck. Also, the Liverpool tool? Lifesaver. I showed my mom how to use it last week. She’s 71, on three meds, and now checks every new supplement. That’s the kind of empowerment we need-not fear, not jargon, just clear tools. Thank you.
Interesting how we treat antivirals like magic bullets but ignore the body’s entire ecosystem. You’re not just fighting a virus-you’re negotiating with enzymes, pumps, and gut bacteria that have been evolving for millions of years. And we think we can outsmart them with a pill and a checklist? Maybe. But we’re still playing catch-up. The real future isn’t better drugs. It’s better listening. Ask patients what they’re taking. Even the ‘harmless’ stuff. Even the tea their grandma swears by. That’s where the real data lives.