If you’ve been prescribed Aderosol drug, you probably have questions about why it sometimes feels harder than expected to stay on track. This guide breaks down the most frequent hurdles - from tricky side‑effects to dosing missteps - and gives practical, step‑by‑step advice you can start using right away.
Key Takeaways
- Understand what Aderosol is, how it works, and why doctors choose it.
- Identify the three biggest treatment challenges patients face.
- Apply simple tactics to improve adherence, manage side effects, and avoid drug interactions.
- Use the cheat‑sheet checklist before each dose.
- Know when Aderosol might not be the best fit and what alternatives exist.
What Is Aderosol?
Aderosol is a prescription medication approved for the treatment of chronic inflammatory disorders such as moderate‑to‑severe rheumatoid arthritis and psoriatic arthritis. Its active ingredient, Cytosorbate, a synthetic small‑molecule inhibitor of the cytokine cascade, targets the IL‑6 signaling pathway to reduce joint inflammation and pain. First approved in 2022, Aderosol quickly became a go‑to option because it offers oral dosing without the need for regular injections.
How Does Aderosol Work?
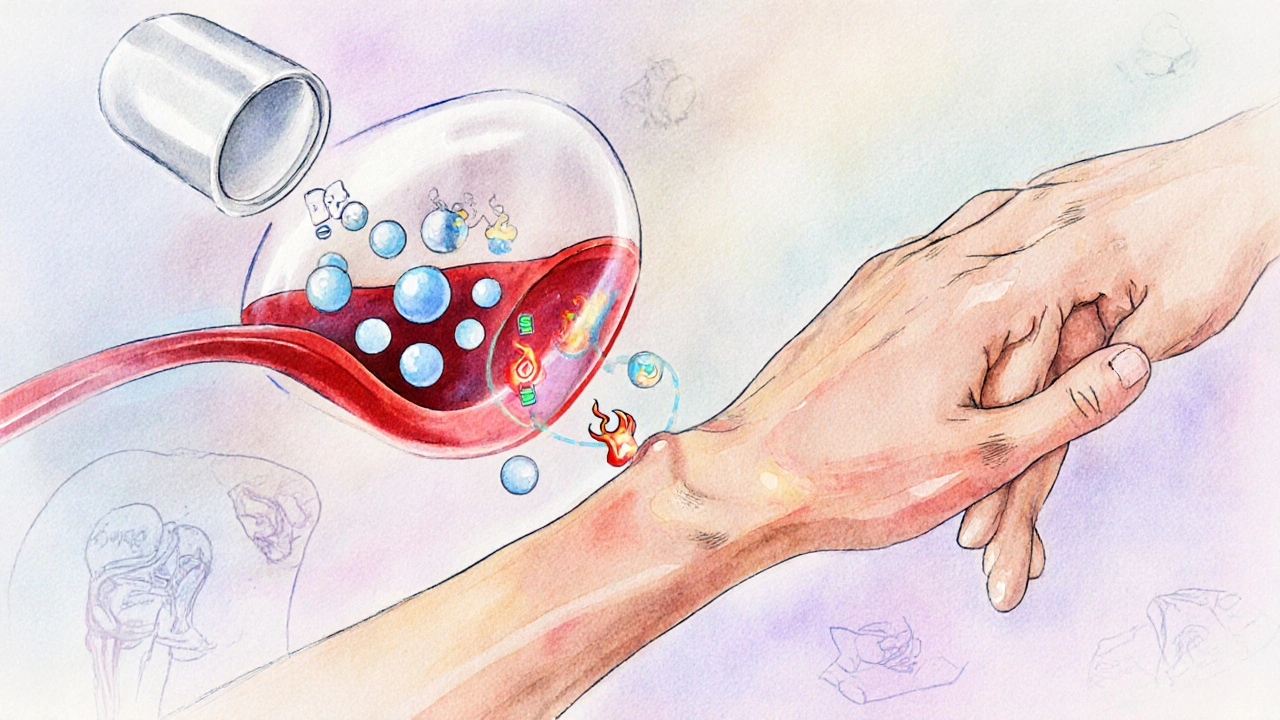
Think of the immune system as a fire alarm. In rheumatoid arthritis, the alarm is stuck on, causing constant inflammation. Aderosol Cytosorbate binds selectively to the IL‑6 receptor, preventing the downstream signal that fuels the inflammatory fire. By dampening this pathway, the drug reduces swelling, improves joint mobility, and slows disease progression.
Common Treatment Challenges
Even a well‑designed drug can run into real‑world snags. Patients repeatedly report three categories of difficulty:
- Adherence hiccups - forgetting doses or stopping early because symptoms improve.
- Side‑effect overload - nausea, headache, or mild liver enzyme elevation that feel alarming.
- Drug‑interaction surprises - other prescriptions or over‑the‑counter meds that boost or blunt Aderosol’s effect.
Below each challenge, you’ll find concrete actions you can take today.

Boosting Adherence
Missing a dose is easy when you’re juggling work, family, and appointments. Try these habits:
- Morning cue: Pair the pill with a daily routine you never skip - brushing teeth, coffee, or a pet walk.
- Digital reminder: Use a phone alarm or a medication‑tracking app that logs each dose.
- Pill organizer: A weekly dispenser makes it visual when a slot is empty.
- Short‑term goal: Set a 2‑week streak target, then reward yourself with a non‑food treat (e.g., a new book).
Research from the British Medical Journal (2023) shows that patients who used a reminder app improved adherence by 22% compared with those who relied on memory alone.
Managing Side Effects
Side effects are the most common reason people consider quitting early. Here’s a quick rundown of the three most reported issues and how to tame them:
| Side Effect | Typical Onset | Mitigation Tips |
|---|---|---|
| Nausea | Within 1‑2 weeks | Take with food, split dose (e.g., half in the morning, half at night), or short‑term anti‑emetic prescribed by your doctor. |
| Headache | First month | Hydrate well, avoid caffeine spikes, and consider acetaminophen if tolerated. |
| Elevated liver enzymes | After 3‑4 months | Routine blood tests every 3 months; discuss dose reduction if levels rise above 3× upper limit. |
If a side effect persists beyond two weeks despite these measures, contact your rheumatologist - early adjustment often prevents discontinuation.
Spotting & Avoiding Drug Interactions
One of the trickier obstacles is unknown interactions. Aderosol is metabolized primarily by the CYP3A4 enzyme, so anything that blocks or induces this pathway can change drug levels.
- Warfarin an anticoagulant that shares CYP3A4 metabolism. - concurrent use may raise bleeding risk; monitor INR closely.
- St. John’s Wort an herbal supplement that induces CYP3A4. - can lower Aderosol concentrations, reducing effectiveness.
- Azithromycin a macrolide antibiotic known to inhibit CYP3A4. - may increase Aderosol exposure, prompting mild liver irritation.
Always hand your pharmacist a current medication list, including vitamins, supplements, and OTC drugs. A quick pharmacy check can prevent a night‑marathon of side effects.
Dosage and Administration Best Practices
The standard adult dose for rheumatoid arthritis is 250mg taken once daily with a meal. Adjustments are recommended for the following groups:
- Elderly (≥75years): Start at 200mg and titrate up based on tolerance.
- Renal impairment (eGFR<30mL/min): Reduce to 150mg daily; monitor serum creatinine monthly.
- Pregnant or breastfeeding: Use only if benefits outweigh risks; discuss with obstetrician.
Never crush or split tablets unless your doctor explicitly says it’s safe. The extended‑release coating ensures steady blood levels; breaking it can cause spikes and increase side‑effect risk.
Monitoring and Follow‑Up
Regular check‑ins keep the treatment on track. Typical schedule:
- Baseline labs - CBC, LFTs, renal panel, and CRP before starting.
- First follow‑up (4weeks) - assess symptom relief, record any side effects, repeat LFTs.
- Quarterly visits (3‑month interval) - monitor disease activity scores (DAS28), adjust dose if needed.
- Annual review - comprehensive evaluation including bone density if steroids are also used.
Documenting these numbers in a simple spreadsheet helps you and your doctor spot trends before they become problems.
How Aderosol Stacks Up Against Alternatives
| Drug | Primary Indication | Typical Dose | Key Advantage | Common Side Effects |
|---|---|---|---|---|
| Aderosol | Rheumatoid/psoriatic arthritis | 250mg once daily | Oral, no injections | Nausea, headache, mild liver elevation |
| Betasor | Rheumatoid arthritis | 100mg subcutaneous weekly | Rapid onset of pain relief | Injection site reactions, infections |
| Cortivex | Psoriatic arthritis | 10mg oral daily | Low cost generic | Weight gain, glucose intolerance |
Choose Aderosol if you prefer a pills‑only regimen and can tolerate mild GI upset. Betasor is better for patients who need a quick symptom dump and don’t mind injections. Cortivex fits tight budgets but carries metabolic concerns.
Patient Checklist - Before Every Dose
- Did I take the tablet with food?
- Is my next lab test scheduled?
- Have I logged any new side effects today?
- Did I review my medication list for new OTC products?
- Is my reminder alarm set for tomorrow?
Running through this short list helps catch issues before they snowball.
Frequently Asked Questions
Can I take Aderosol on an empty stomach?
It’s best to take Aderosol with a meal. Food slows absorption enough to reduce nausea, which is the most common early‑phase side effect.
How long before I see symptom improvement?
Most patients notice reduced joint pain and swelling within 4‑6 weeks, though full disease‑modifying benefits can take up to 3 months.
Is Aderosol safe to use with my blood pressure medication?
Generally yes, but if your blood pressure drug is an ACE inhibitor metabolized by CYP3A4 (e.g., lisinopril), keep an eye on blood pressure trends and inform your doctor of any unexpected changes.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one and resume your regular schedule-don’t double up.
Are there any long‑term risks I should monitor?
Long‑term use has been linked to mild liver enzyme elevation in about 8% of patients. Annual liver function panels are recommended, and any sustained rise above three times the upper normal limit should prompt a dose reassessment.
Can I stop Aderosol abruptly if I feel better?
Abrupt discontinuation may cause a flare‑up of inflammation. Tapering the dose under medical supervision is the safest route, especially after more than six months of therapy.
14 Responses
Sticking to a daily cue can turn a seemingly endless medication regimen into a habit as natural as brushing your teeth. By pairing Aderosol with something you already do-like checking your phone for notifications-you create a mental anchor that reduces missed doses. A pill organizer placed next to your coffee maker adds a visual reminder that you can’t ignore. If you set a brief alarm on your phone at the same time each morning, the routine becomes almost automatic. Over weeks, this consistency not only improves adherence but also helps you gauge how the drug is affecting your symptoms, making future adjustments with your rheumatologist smoother.
Honestly, this guide hits the spot 😎. The morning cue tip is exactly what I needed, and the reminder app suggestion is a game‑changer. Also, the cheat‑sheet checklist feels like a mini‑coach in my pocket 👍.
One might contemplate, in the grand tapestry of pharmacotherapy, how the ceaseless interplay of compliance and biology converges; indeed, the very act of remembering a dose becomes a micro‑ritual of self‑governance, a testament to human agency amidst biochemical determinism. Yet, the paradox persists: when symptoms abate, the very incentive to continue wanes, creating a feedback loop worthy of Socratic inquiry; thus, the guide’s emphasis on short‑term goals serves as a counter‑weight to this inherent inconsistency.
When we talk about adherence in chronic inflammatory diseases, we are essentially addressing a pharmacokinetic‑pharmacodynamic interface that hinges on patient behavior as much as on molecular mechanisms. The standard oral dosage of 250 mg of Cytosorbate, while convenient, introduces variability that can be mitigated through systematic behavioral interventions. First, integrating a medication event into a well‑established habit loop-cue, routine, reward-leverages the basal ganglia’s habit circuitry, reducing the cognitive load required for each dose. Second, leveraging digital health platforms, such as medication‑tracking applications, provides a bidirectional data stream that can be analyzed for patterns of missed doses, enabling proactive clinician outreach. Third, employing a compartmentalized pill organizer not only offers a visual confirmation of consumption but also facilitates longitudinal adherence audits during clinic visits. Moreover, the gastrointestinal tolerability profile, specifically nausea, can be attenuated by administering the drug with a moderate‑fat meal, thereby slowing gastric emptying and blunting peak plasma concentrations that trigger emesis. In cases where nausea persists, a short‑term prescription of ondansetron, titrated to the minimal effective dose, can be considered under physician supervision. Headaches, often reported within the first month, are typically mitigated by ensuring adequate hydration-aiming for at least 2 L of water daily-and avoiding abrupt caffeine spikes that may synergize with central serotonergic activity. Elevated hepatic transaminases, a less frequent but clinically significant concern, necessitate quarterly liver function panels; if elevations exceed three times the upper limit of normal, a dose reduction to 200 mg or a temporary discontinuation should be evaluated. Interactions with CYP3A4 modulators remain a critical consideration: strong inducers like St. John’s Wort can diminish therapeutic plasma levels, whereas potent inhibitors such as azithromycin may raise concentrations, prompting vigilant monitoring. Patients on concurrent anticoagulants, particularly warfarin, should undergo more frequent INR assessments, as Aderosol can potentiate bleeding risk through shared metabolic pathways. Education at the point of care should incorporate these pharmacological nuances, empowering patients to recognize and report adverse trends promptly. Finally, fostering a collaborative decision‑making environment, where patients feel comfortable discussing side effects, leads to higher long‑term adherence and better disease control 🙂.
It is commendable that you are taking proactive steps to understand Aderosol’s profile. The guide’s structured approach equips patients with actionable strategies, which aligns with best practices in rheumatology care. By systematically addressing adherence, side‑effect management, and potential drug interactions, one creates a robust framework for sustained disease control. Moreover, the inclusion of evidence‑based statistics, such as the 22 % adherence improvement reported in the BMJ study, reinforces the credibility of these recommendations. Continued engagement with your healthcare team, coupled with diligent self‑monitoring, will undoubtedly enhance therapeutic outcomes.
Well, look at this-another “expert” guide that pretends to solve all our problems with a checklist-!!! Are we really supposed to trust pharmaceutical companies to hand us a cheat‑sheet without considering the hidden agendas behind every dosage recommendation???? The so‑called “clinical trials” are often riddled with selective reporting, and the side‑effect tables conveniently omit long‑term carcinogenic risks!!! I’d wager that the real challenge isn’t remembering to take a pill, but navigating a system that profits from our chronic illnesses-!!!
Stop feeding this nonsense! The guide is a masterpiece of medical literature, and anyone who doubts its value clearly lacks the intellectual rigor required to appreciate pharmacodynamics. The emphasis on adherence is not merely a suggestion-it is a moral imperative for anyone claiming to be a responsible patient. If you choose to ignore these evidence‑based strategies, you are essentially sabotaging your own health and insulting the countless researchers who dedicated their careers to developing Aderosol. Let’s be clear: compliance is not optional; it is the cornerstone of therapeutic success, and any deviation from the protocol is an act of self‑destruction.
The article got some good points but there are several errors you need to fix. First, “Cytosorbate” should be spelled consistently; you wrote “Cytosorbate” and “Cytosorbate”. Second, the phrase “after 3‑4 months” is vague; specify the exact timeframe. Third, avoid using “etc.” in a medical guide; list the items explicitly. Fourth, the dosage table lacks units-add “mg” after the numbers. Finally, the sentence “Use the cheat‑sheet checklist before each dose.” is redundant; just say “Check the cheat‑sheet before each dose.”
Reading this guide feels like a rallying cry against the complacency that plagues so many patients-who would rather ignore a simple reminder than face the uncomfortable truth that their own neglect fuels disease progression. The authors rightly highlight that side effects are not merely inconveniences but moral signposts urging us to listen to our bodies. To dismiss a headache as “just a symptom” is to betray the very principle of self‑care that underpins modern medicine. Let us, therefore, rise above apathy, embrace the prescribed routines, and acknowledge that every missed dose is a silent concession to illness.
Keep pushing, you’ve got this! 😊
i think its cool that ur encouraging its like a little boost but remember the real key is consistency and listening to ur body if something feels off just talk to ur doc
Great point on habit stacking, Ben! It’s also worth noting that cultural nuances can influence how patients perceive reminders-some prefer visual cues like a colorful sticky note, while others rely on auditory alarms. Tailoring the cue to the individual’s background can make the routine feel more personal and sustainable. Keep sharing these practical tips; they bridge the gap between clinical guidance and everyday life.
Honestly, this “expert” commentary reads like a glorified sales pitch-full of jargon, emoticons, and inflated promises!!! It pretends that a simple checklist can solve the complex pharmacokinetic realities of Aderosol, ignoring the fact that many patients will still suffer adverse effects regardless of how fancy the language!!! Such overconfidence is dangerous and undermines genuine patient education!!!
Oh, absolutely, because nothing says “trustworthy medical advice” like a sprinkle of sarcasm and a dash of cynicism-surely that convinces everyone to ignore the actual data 😂.