Acute Kidney Injury (AKI) doesn’t announce itself with a siren. It creeps in quietly-maybe after a bad bout of food poisoning, a sudden drop in blood pressure, or even after a routine CT scan. One day you feel fine; the next, your legs are swollen, you’re exhausted, and your urine has slowed to a trickle. By the time symptoms show up, your kidneys may already be struggling. AKI isn’t just a lab value-it’s a medical emergency that can turn deadly in hours if missed.
What Exactly Is Acute Kidney Injury?
AKI means your kidneys suddenly lose their ability to filter waste from your blood. This isn’t a slow decline like chronic kidney disease. It happens fast-within hours or days. The old term, acute renal failure, is outdated. Doctors now say injury because even small drops in kidney function can trigger serious problems. The current standard, set by KDIGO in 2012, defines AKI by two things: a rise in serum creatinine (a waste product your kidneys normally clear) or a drop in urine output.
For example, if your creatinine jumps by 0.3 mg/dL in just 48 hours-or rises 50% from your normal level-that’s AKI. Even if you’re still peeing normally, your kidneys might be failing. About 22% of cases are found only because someone had routine blood tests. No symptoms. No warning. Just a lab result that says, “Something’s wrong.”
How Do You Know If You Have It?
Symptoms vary wildly. Some people feel terrible. Others feel fine. The most common sign is less urine-under 400 mL a day (oliguria), or even under 100 mL (anuria). But don’t assume you’re safe just because you’re peeing. In cases of urinary blockage, your kidneys might still produce urine, but it can’t get out.
Other signs include:
- Swelling in your legs, ankles, or feet (fluid retention in 68% of cases)
- Shortness of breath from fluid in the lungs (42% of hospitalized patients)
- Extreme fatigue (75% of cases)
- Nausea or vomiting (58%)
- Confusion or drowsiness, especially in older adults (33%)
- Flank pain (back pain just below the ribs, in 27% of cases)
- Chest pain from inflammation around the heart (15%)
And here’s the scary part: if you’re in the hospital-especially in intensive care-you might not feel any of this. That’s why doctors check creatinine every 24 to 48 hours for high-risk patients. Waiting for symptoms is too late.
Why Did This Happen? The Three Big Causes
AKI doesn’t happen randomly. It has a clear cause-and knowing which one is key to fixing it. There are three main types:
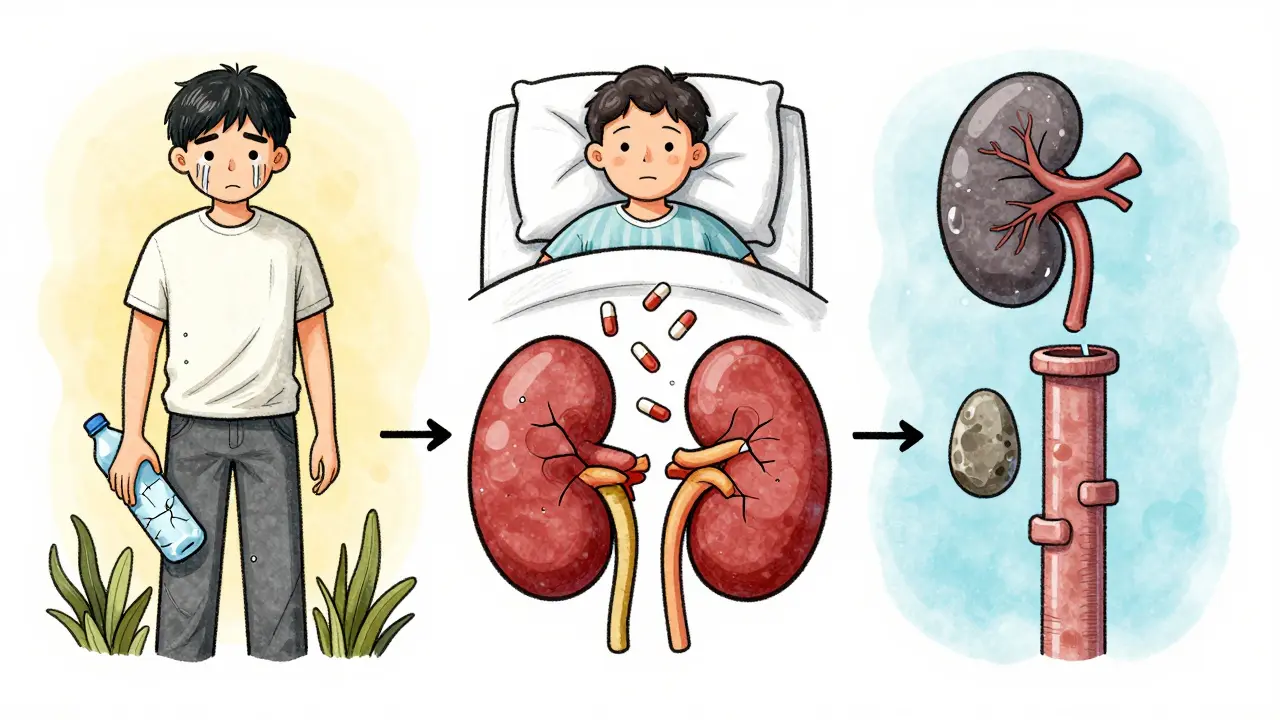
1. Prerenal (60-70% of cases)
Your kidneys aren’t damaged-they’re just not getting enough blood. Think of it like turning down the water pressure to a faucet. Causes include:
- Severe dehydration from vomiting, diarrhea, or not drinking enough (15-20% of community cases)
- Low blood pressure from infection (sepsis), heart failure, or heavy bleeding
- Medications like NSAIDs (ibuprofen, naproxen) or blood pressure drugs that reduce kidney blood flow
Fixing this is often simple: give fluids. A 500-1000 mL IV saline bolus can turn things around in 24-48 hours. But if you wait too long, the lack of blood flow can damage the kidney tissue itself.
2. Intrarenal (25-35% of cases)
This is direct damage inside the kidney. The most common cause? Acute tubular necrosis (ATN)-when the tiny filtering tubes in the kidney die. This often follows:
- Severe infection or shock
- Nephrotoxic drugs: antibiotics like gentamicin, contrast dye used in CT scans (5-15% of cases), or even high doses of painkillers
- Autoimmune conditions like glomerulonephritis or lupus
Unlike prerenal AKI, fluids won’t fix this. You need to stop the poison, treat the infection, or use immune-suppressing drugs. Recovery takes weeks, and not everyone gets back to full function.
3. Postrenal (5-10% of cases)
This is a plumbing problem. Something is blocking urine from leaving your body. Common causes:
- Enlarged prostate in men over 60 (65% of obstructive cases)
- Kidney stones blocking both ureters
- Tumors pressing on the urinary tract
Ultrasound is the go-to test here-it can spot swelling in the kidneys and show if urine is backed up. Relief? A stent or catheter. Once the blockage is gone, kidneys often bounce back fast. But if it’s left too long, permanent damage can happen.
What Happens If It’s Not Treated?
Untreated AKI doesn’t just stay stuck-it gets worse. Fluid builds up, leading to pulmonary edema. Potassium rises dangerously high (hyperkalemia), which can stop your heart. Your blood becomes too acidic (metabolic acidosis). You can develop pericarditis, a painful inflammation around the heart.
And even if you survive, the damage lingers. One in five AKI survivors develops chronic kidney disease within a year. Each episode of AKI raises your five-year risk of needing dialysis by more than eight times. The mortality rate? Up to 37% if you’re in the ICU. If you need dialysis, it’s closer to 50%.
How Is It Diagnosed?
Doctors don’t guess. They measure:
- Serum creatinine: The gold standard. A rise of 0.3 mg/dL in 48 hours or 50% over 7 days confirms AKI.
- Urine output: Less than 0.5 mL per kg of body weight per hour for 6 hours.
- BUN (blood urea nitrogen): Often high, but can be misleading if you’re dehydrated.
- FeNa (fractional excretion of sodium): Under 1% suggests prerenal; over 2% suggests kidney damage.
- Renal ultrasound: Used in 85% of cases to rule out blockages and check kidney size.
Emerging tools are changing the game. Tests for biomarkers like NGAL can detect AKI 24-48 hours before creatinine rises. The NICE guidelines now recommend these in high-risk patients. AI systems are also being tested to predict AKI before it happens-by analyzing patterns in your vital signs and lab history.
How Is It Treated?
Treatment isn’t one-size-fits-all. It depends entirely on the cause.
- Prerenal: IV fluids. Fast. Often works in under 2 days.
- Intrarenal: Stop the offending drug. Treat infection. Use steroids for autoimmune causes. Plasmapheresis for rare conditions like HUS.
- Postrenal: Remove the blockage. A stent in the ureter fixes 90% of cases within hours.
If things get severe-high potassium, fluid in the lungs, or acidosis-you may need dialysis. About 5-10% of hospitalized AKI patients need it. For ICU patients, continuous renal replacement therapy (CRRT) is common. It’s slower and gentler than traditional dialysis, better for unstable patients.
Here’s the truth: early action saves kidneys. If you catch AKI at Stage 1 (mild), recovery chances are over 70%. At Stage 3 (severe), even with treatment, only 20-30% fully recover.

Can You Recover Fully?
Yes-but it’s not guaranteed. Recovery depends on three things: how bad it was, how fast you got help, and your baseline health.
- Prerenal AKI: 70-80% recover fully in 7-10 days if treated early.
- Intrarenal AKI: 40-60% recover, but it takes weeks. Some are left with permanent damage.
- ATN with prolonged low urine output: Only 20-30% recover fully if it lasts more than two weeks.
Factors that make recovery harder:
- Age over 65 (recovery rate drops 35%)
- Pre-existing kidney problems (eGFR under 60)
- AKI lasting more than 7 days
- Needing dialysis (only 25% recover full function by 3 months)
And recovery isn’t just about creatinine numbers. Many survivors say they feel “kidney fatigued” for months-exhausted, unable to walk far, mentally drained. One patient on a support forum said: “Even after my creatinine returned to normal, I couldn’t walk 50 feet without collapsing. The fear that I’d need dialysis forever was worse than the illness.”
What Happens After You Leave the Hospital?
Most people think AKI is over when they’re discharged. It’s not.
Forty-five percent of survivors need to see a kidney specialist within six months. Twenty-three percent develop chronic kidney disease within a year. That’s why follow-up is non-negotiable.
Your doctor should check:
- Creatinine and eGFR at 1, 3, and 6 months
- Urine protein levels
- Blood pressure
- Medications that might harm your kidneys
And you need to stay hydrated, avoid NSAIDs, and watch your salt and protein intake. No more “I’ll just take an Advil for my headache.”
What’s Next for AKI?
Research is moving fast. The STARRT-AKI trial found that starting dialysis earlier in severe cases cut 90-day death rates by 9%. New biomarkers like TIMP-2 and IGFBP7 can predict AKI 12 hours before symptoms show-especially in ICU patients. AI tools are being trained to spot AKI risk by analyzing your electronic health record before you even feel sick.
The goal? Prevent it before it starts. If we can predict AKI 12-24 hours ahead, we can give fluids, stop bad drugs, or adjust treatments before damage occurs. The Kidney Precision Medicine Project estimates this could reduce AKI cases by 20-30%.
For now, the message is simple: if you’re at risk-elderly, diabetic, on multiple meds, recently hospitalized-ask for your creatinine to be checked. Don’t wait for swelling or fatigue. A simple blood test can save your kidneys-and your life.
13 Responses
Yo, this post is spot on but everyone skips the real issue: hospitals don't test creatinine proactively unless you're in ICU. I'm from Lagos, and my uncle got AKI after a fever-he was discharged with 'just dehydration' and ended up on dialysis three weeks later. No one checked his labs. This isn't just medical-it's systemic neglect in low-resource settings.
AKI isn't 'sudden'-it's the inevitable result of lazy clinical practice. If you're on NSAIDs, statins, and ACE inhibitors, and you're over 60, you're already on a countdown. Stop pretending it's mysterious. It's pharmacology 101.
Really appreciate this breakdown. I'm a med student in Delhi, and we see so many cases from dehydration + over-the-counter painkillers. One thing missing: how do we educate people who don't know 'creatinine' means anything? Maybe community health workers with simple visuals-like a kidney filter with clogged pipes-could help. We need grassroots awareness, not just hospital protocols.
It’s wild how we treat kidneys like spare parts. We’ll go to yoga for our spine, meditate for our mind, but ignore the organ that literally keeps our chemistry balanced. AKI isn’t just a disease-it’s a mirror of how we treat our bodies: reactive, not preventive. We wait for the alarm to blare before we fix the wiring.
The KDIGO criteria are robust, but their implementation remains inconsistent across institutions. A 0.3 mg/dL rise in creatinine is statistically significant, yet many clinicians still rely on subjective assessments of volume status. This discrepancy undermines early intervention. Standardization of protocols is not optional-it is imperative.
THIS. I’m a nurse in Chicago. We had a guy come in with no symptoms, just a weird lab result-creatinine up 50%. He was a diabetic on metformin and ibuprofen daily. We started fluids, pulled the NSAIDs, and he was out in 3 days. If we’d waited for swelling or fatigue? He’d be in dialysis. Early = easy. Late = life-changing. Spread this word.
So let me get this straight-you’re telling me the same doctors who told me my 'stress' was causing my headaches are now the ones who 'missed' my kidney failure? 😂 Maybe stop prescribing me 800mg ibuprofen for 'migraines' and start listening? Also, why is it always 'old people' who get this? Oh right, because we're the ones who still trust the system.
Contrast dye causes AKI? Shocking. Next you'll tell me smoking causes lung cancer. People take NSAIDs like candy and wonder why they're in the hospital. It's not a mystery-it's negligence wrapped in a white coat. Stop acting surprised. You knew.
This is a clinically comprehensive and exceptionally well-referenced overview. The integration of KDIGO guidelines with real-world prevalence data, coupled with the emphasis on longitudinal follow-up, underscores the necessity of a multidisciplinary approach to post-AKI care. I commend the author for highlighting the psychosocial burden-a dimension often omitted from biomedical discourse.
i read this whole thing and my head hurts 😭 i just wanted to know if i should stop taking tylenol for my back pain. can someone just tell me yes or no? also why is everyone talking about creatinine like its a person??
They say AKI is from meds or dehydration but what if it's the water? The fluoridated tap water? The glyphosate in our food? The 5G towers? They're testing creatinine to distract you from the real toxins-big pharma and the government are hiding the truth. They don't want you to know kidneys can heal naturally with lemon water and moon cycles
What if AKI isn't a disease at all? What if it's your body's way of saying: 'I'm tired of being treated like a machine.' You're on 12 pills, you're glued to your screen, you're drinking diet soda like it's water-your kidneys are staging a rebellion. This isn't medicine-it's a spiritual crisis wearing a lab coat. Wake up. Your organs are begging you.
Incorrect. The term 'acute renal failure' isn't outdated-it's more precise. 'Injury' implies reversible damage, but many cases result in permanent fibrosis. The KDIGO criteria overdiagnose mild cases that resolve spontaneously. This pathologizes normal variation. Stop medicalizing every creatinine fluctuation.